Research Article
Volume 2 Issue 5 - 2019
Improving the Effectiveness of Reparative Regeneration in Children and Adolescents with the Disease Legg – Calve – Perthes
1Regional Children's Clinical Hospital, Ivanovo, Russia
2Ivanovo state medical Academy, Ministry of health of Russia, Ivanovo
3Clinic of Ivanovo state medical Academy, Ministry of health of Russia, kohma
2Ivanovo state medical Academy, Ministry of health of Russia, Ivanovo
3Clinic of Ivanovo state medical Academy, Ministry of health of Russia, kohma
*Corresponding Author: IL Lobov, Regional Children's Clinical Hospital, Ivanovo, Russia.
Received: April 01, 2019; Published: April 09, 2019
Abstract
Introduction: The cause of Legg-calve-Perthes disease (blcp) is not fully understood. Attempts to increase the strength of the bone tissue of the femoral head with the help of known conservative therapeutic measures are still not effective. We believe that improving the quality of reparative regeneration is the main task of an orthopaedist.
Objective: Тhe study was an assessment of the use of the study was to assess the recovery of bone strength using osteochondropathies in children with (blcp).
Materials and Methods: 65 patients at the age of 3-12 years were examined. We evaluated and compared the main static-dynamic, radiological, computer tomographic parameters with the results in the opposite hip joint. The changes in laboratory parameters in each stage of the disease were determined.
Results: Revealed the marked decrease in bone density in the II - III stages BLK all 65 patients in the femoral head of more than 100 – 200 specific densitometric Hounsfield units and an increase in β-Cross Laps in 20 children is more than 5.3 ng/ml (p < 001) compared to the norm of 0.3 – 0.57. In 31 children (47.7 per cent), low physical development, and hypo function of the proximal growth zone of the femur (PSRBC) under the age of 8 years between Catterall II after injection of IV stage BLK came after 12 – 18 months (Stulberg).
The structure and form of the proximal epiphysis of 24 children (36.9%) under the age of 8 years between Catterall III with destructive variant of functioning PSRBC restored after 18-24 months. In addition, bone destruction index (Catterall II – III) significantly decreased to physiological norm in 16 patients after 6 months. In 10 adolescents (15.4%) older than 8 years with a hypersthenic Constitution and dystrophic variant of the functioning of PZRBC (Herring B), the recovery stage ended by 24-30 months, and a decrease in the level of β – CGS Laps in 4 patients to the norm was recorded after 12 months. The restoration of the sphericity of the femoral head in all patients depended on the synchronicity of the functioning of the individual portions PSRBC. The main biochemical parameters in all stages of blkp corresponded to physiological norm.
Conclusion: Thus, it can be considered that the injection of osteoprotector is one of the main mechanisms of stimulation of reparative regeneration of bone tissue in patients with blcp and can be recommended in the practice of pediatric orthopaedist.
Keywords: Children; Hip Joint Diseases; Perthes Disease; Reparative Regeneration; Conservative Treatment
Introduction
Legg-calve-pertes disease (blcp) is one of the most common osteochondropathies in childhood. Its etiopathogenesis is not fully understood. In children with blcp in the II – III stages, the process of bone necrosis prevails over regeneration, up to the total destruction of the femoral head. In the IV stage, the power of reparative regeneration is already sufficient to restore the affected head. The absence of congruence of the articular surfaces of the hip joint (TBS) in the stages of recovery and outcome inevitably leads to the development of coxarthrosis and deterioration of quality of life.
In modern literature, the process of osteonecrosis is strongly associated with impaired collagen biosynthesis in the subchondral zone of the affected epiphysis [1-4]. The mechanism of osteoregeneration is not fully disclosed. Typically, the literature describes the most popular methods of stimulation of regeneration of bone tissue. One of them is the appointment of physiotherapeutic procedures (electrophoresis with potassium iodide, calcium chloride, phosphorus and sulfur) [5-7]. The penetration depth of trace elements is not great 0.5 – 1.0 cm, and their concentration is not enough for a full restoration of the proximal epiphysis. Another of the known options for strengthening the strength of bone tissue is the appointment of angioprotectors and venotonics (trental, no-shpa, kurantil) orally.
Their pharmacodynamics allows to improve hemodynamic and rheological properties of blood in vessels surrounding the femoral neck [8-9]. In addition, they are used in solutions (nicotinic acid and eufillin) in the form of electrophoresis on the lumbosacral region, which provides a focused effect on the vascular network of TBS. However, the normalization of blood circulation, combined with the physiotherapy effect does not guarantee the destruction of the focus of osteonecrosis, and the duration of the disease is not significantly reduced. Relief of vasoconstriction is also possible when prescribing drugs with antioxidant effect (Mexidol) intramuscularly and physiotherapy [10].
To increase the effectiveness of bone regeneration, drugs regulating calcium-phosphorus metabolism (osteogenon, oxidevit, alpha - D3 — TEVA) and osteo-chondroprotectors (teraflex, Dona, calcimax) are used orally [11-12]. Their pharmacological effect is activation of activity of cells of creators - osteoblasts and inhibiting osteoclasts. However, the time of transportation of active metabolites with this route of administration increases, and the rate of regeneration is reduced by natural theft to other target organs. A good result is achieved only in young patients, in the early stages of the disease and with the volume of the focus of necrosis not more than 50%.
In addition, they are contraindicated in patients with diseases of the genitourinary system. An increase in the mineralization of the affected proximal epiphysis is also possible with the help of bisphosphonates (zoledronic acid solution) intravenously [13-14]. Its pharmacological properties provide inhibition of osteoclast resorption process and accelerate osteoblastic activity of cells. They allow to increase the share of mineralization of the destroyed epiphysis in the III stage of blcp by 72% in 24-36 months.
However, its use in children is limited due to premature hypercalcemia in various parts of the skeleton and parenchymatous organs. Improvement of articular cartilage metabolism in TBS is also achievable with intraarticular or periarticular injection (rumalon, vitreous, propolis, perftoran) in solution [15-16], but their pharmacological potential is not sufficient to restore the destroyed bone tissue. It should be recognized that this method of delivery of the drug is the shortest, most promising and long-term. In the literature, most often all of the above methods of stimulation of osteoregeneration, except bisphosphonates, are used in a complex.
The main disadvantage of complex therapy is the lack of evidence of the exact pharmacological effectiveness of each drug separately. Extremely rare publication, is dedicated to changing laboratory diagnostics, bone density, disturbance in PSRBC [17, 18]. There is no x-ray and tomographic systematization of anatomical and functional state depending on the Constitution of the patient. There are not enough reports about the influence of pathophysiological action of femoro - acetabular impingement (FAI) on the shape and structure of the articular surfaces of TBS. Osteoprotegerin is available in pharmaceutical form solution for injection. Their main pharmacological action is on the one hand the suppression of aseptic inflammation, and on the other stimulation of reparative regeneration of bone and cartilage. Drugs can be applied as intra-articular, periarticular and intramuscular. Therefore, the aim of the study was to assess their effect on reparative regeneration in children with blcp.
Material and Methods
We examined 65 patients aged 3–12 years, who were treated in the Department of pediatric orthopedics 2003 – 2016. Boys were 60 (88.8%), and girls – 5 (11.2%). At the beginning of the study, we obtained the voluntary consent of parents of children and adolescents under 15 years of age with this disease to participate in the study and the processing of their personal data. The defeat of the right TBS was 47.7% (31 cases), the left – 44.6% (29 cases), and both TBS – 7.7% (5 cases). Clinical examination included the study of the main static-dynamic indicators of orthopedic status at admission of the patient and at each stage of the disease. Static values: relative length of both lower extremities, absolute length of hips and shins, as well as their circumferences were measured in centimeters, and dynamic in degrees, using the nomenclature goniometer (SFTR) in comparison with healthy TBS.
To identify the radiological stages of the disease, the classification of S. A. Reinberg (1964) in standard projections was used. The increase in the degree of osteonecrosis in patients up to 8 years was judged by Catterall classification (1980), where its I degree = 25%, II – 50%, III – 75%, IV – 100%, and in patients older than 8 years by Herring., et al. (1991): A — 25%; B — 50%; C — 100%. Restoration of the shape and structure of the affected epiphysis was determined by the classification of Stulberg., et al. (1981) as modified by Neyt., et al. (1999), where A is the spherical shape of the femoral head; B is mushroom-shaped; C is flat. The formation of the FAI was determined radio graphically in the anterior-posterior projection. Its main features were considered to be the asymmetry of the interversal line over 1.0 cm, a decrease in the angle formed between the Sadofieva line and the tangent to the vertex of the acetabulum more than 15° and a step bend of the Shenton line more than 5mm. the Interversal line connects two points of the vertices of the large spits of both TBS.
The Sadofieva line crosses the middle of the femoral neck and connects the centers of the femoral head and acetabulum. Tangent to it is held from the center of the femoral neck to the top of the acetabulum. The Shenton line is drawn against the lower surface of the upper branch of the pubic bone and the medial surface of the femoral neck. It normally has a smoothly-curved in nature, which shows preservation of normal anatomy. An increase in the ledge-like deformation of more than 5 mm indicated a violation of the anatomical relations in the joint (Figure 1). Classification was used to identify variants of x-ray anatomy and functioning disorders [17].
Deviations PSRBC was assessed according to three criteria: height, width of the growing zone and the uniformity of areas of preparative calcification, compared to the other anatomical structure. The main indicator of the norm of its height and width was considered their uniformity throughout. The zone of drug calcification should be distinct, with a uniform optical density. About hypothyroidism PSRBC judged by the straightness of its outlines, reducing the height, width and narrowing areas of preparative calcification in comparison with indicators of the opposite of TBS.
Height increasing PSRBC, with its uneven contours and heterogeneity of structure of areas of preparative calcification indicated a degeneration growing zone. The characteristic signs of destruction PSRBC considered the inequality in the heights "star" sclerosis, and A V – shaped deformation area of growth, the graininess of the contours of preparative area of calcification without defects. To calculate the magnitude distribution, the location of the volume of osteonecrosis, the depth of the destruction of portions PSRBC, speed of regeneration, as well as the height of the articular cartilage of the femoral head (CHGBK) and its defects used spectral computed tomography (SCT) study on "Brilliance – 6" firm "Philips", the Netherlands (slice thickness 1 mm), in three-dimensional modeling.
The magnitude of the prevalence of osteonecrosis was calculated in the frontal plane, taking the femoral head for a circle. Using the geometric scheme according to the method [19], with its division into 14 sectors. The calculation of its distribution was as follows: 1–3 sectors = 25%; 4–6 = 50% (Subtotal defeat); over 8 = 75 % - total, while their total amount was 100%. In addition, this technique allowed to establish the topographic location of osteonecrosis to the anatomical surfaces of the thigh (Figure 2 and 3). The volume of osteonecrosis was determined in the sagittal plane, taking the proximal epiphysis of the femur as a geometric figure – a hemisphere [19]. The calculation was made by the formula with a given value of the hemisphere and its height in cubic millimeters (mm3). We believe that bone density is a quantitative indicator of the strength of the trabecular system at any point of the child's skeleton, including the proximal epiphysis of the femur. Its calculation was carried out using a local window (Figure 4).
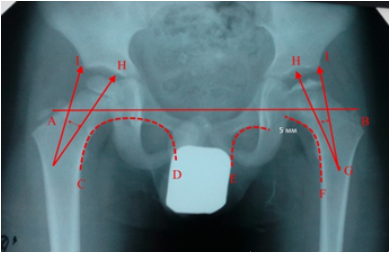
Figure 1: X-ray of TBS in the anterior-posterior projection of patient O., 5 years Diagnosis: "Perthes' Disease on the left, stage III" Catteral III. The change of the spatial geometry. The inter body line (A-B) is synchronous; the Shenton line (E-F) on the affected side is interrupted by 5 mm; the lateralization angle (G-H-I) is reduced.

Figure 2: Sectoral calculation of the distribution and location of osteonecrosis of the femoral head to the anatomical surfaces of the femur by Steppacher.

Figure 3: Determination of the volume of osteonecrosis of the femoral head in children with blcp
Normal density in children 3 to 12 years is in the range of 260 – 320 in specific densitometric Hounsfield units (+ units HU).
Changes in the strength of the trabecular system in the subchondral zone and the rate of regeneration of the affected epiphysis were evaluated in each stage of the disease, comparing them with the indicators of the contralateral side. A reliable indicator of bone mass loss was considered to be over 100 (+ Hu). By means of serial sections in 3D reformation of the refined topography and the extent of destruction of individual portions PSRBC. The estimation of the thickness of CHGBK produced topografichesky, in comparison with the same indicators of the opposite side. Normally, its thickness is 2.0 mm. the Level of bone resorption in 20 patients with blcp in the II – III stages before drug therapy was evaluated by increasing β- Cogs Laps in nanograms per milliliter (ng/ml).
The figures obtained were compared with the age norm of 0.3 – 0.57 ng/ml. blood sampling was performed from the cubital vein. This study has been carried out since 2011. The content of total protein, creatinine and ionized trace elements: calcium and phosphorus was determined by biochemical blood analysis in 65 patients with blcp in all stages of the disease. Normal values varied in the intervals: total protein – 57 - 80 g/l; creatinine – 27 - 62; calcium – 1.12–1.32; phosphorus – 1.29 - 2.26 mmol/l. The stimulation of reparative regeneration was carried out as follows: the cavity of the affected TBS was irrigated with a solution of the drug diluted with 0.5% novocaine (1:3) [20]. Age dosage: 0.1 ml per one year of life of the patient. Maintenance was carried out in sterile conditions, tbs puncture was carried out in typical topographic areas. Intraarticular injection in each patient was performed once using an electron-optical Converter (EOP) (Figure 5)
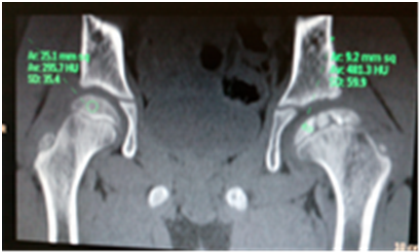
Figure 4: SKT picture of the TBS patient A., age 7 Diagnosis: "Perthes Disease on the left, stage III" Catteral III. Calculation of bone density in units of Hounsfield.

Figure 5: Electron-optical image of the hip joint during intra-articular injection of osteochondroplasty
Re-injection was performed near-articularly, in the same dosages.
A total of 99 therapeutic manipulations were performed, without complications, allergic reactions in patients were not revealed. The effectiveness of drug therapy was judged by reducing the level of bone resorption marker β-Cogs Laps by 25-50% in 16 patients in stage III after 6 months. Reducing the volume of osteonecrosis by 50–100% in the III - IV stages of blcp in 18–24 months, with the restoration of the anatomical and functional state of PZRBC and an increase in bone density in the IV stage of more than 100 units of Hounsfield.
Results and Discussion
Analyzing the results of clinical examination in all 46 patients with stage II blcp, pain in the inguinal region (100%) and gait disturbance (lameness) were revealed in 40 (61.5%) children. The relative length of the affected lower limb in 19 patients (29.3%) younger than 8 years was less than in healthy by 0.5 cm, and in 6 patients older than 8 years it increased to 1.0 cm. the circumference Of the soft tissues of the thigh in all subjects was reduced by 1.0 –1.5 cm, compared with the size of the contralateral side. The amplitude of active movements in the affected TBS was limited due to the deficiency of diversion by 5 - 10° in 20 children (30.8%) and internal rotation of 10 — 15° in all patients. In the remaining 19 (29.3%) children under the age of 8 years, the x-ray pattern corresponded to the III stage of the disease.
The difference of the lengths of the lower limbs consisted of 1.0–1.5 cm, and wasting of the soft tissues of the hips was equal to 2.0 cm abduction Deficit stood at - 15°, external rotation of 10° and internal 15 - 20°. Assessing the x-ray picture in all patients with II – III stages of the disease found that the degree of osteonecrosis they had different. In 46 children in stage II, it was equal to 25% and was already characterized by a change in the trabecular structure in the femoral head in the form of the formation of focused structure less areas. Whereas in 19 patients in the III stage of the disease it occupied 50–75%. Changes in bone strength were determined both in the proximal epiphysis and in the femoral neck in the form of rarefaction areas along its entire width under the mandibular MEMBRANE.
Bone resorption was accompanied by a decrease in the height of the proximal epiphysis, but its sphericity was not disturbed. Intertrochanteric line were symmetrical, and Sadofieva and Shenton had a smooth ride, which is evidence of the congruence of the articular surfaces of TBS. Analysis rentgenograficheskoe state PSRBC in patients with BLK showed diverse changes. This files most often recorded the violation in the form of hypo function of 36 cases (55.4%). Whereas in 20 cases (30.8%) noted destruction, and in 9 (13.8%) revealed its dystrophic violation. We believe that changes detected PSRBC is likely to be associated with the pathogenesis of disease in patients with different physical development. In children with stunting at the onset of the disease, its hypo function was more common, destructive disorders were detected in patients with moderate development, and dystrophic changes were noted in hyperstenics (Figure 6, 7, 8).
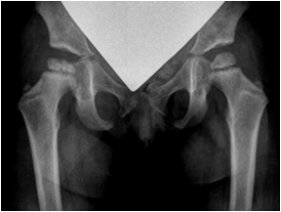
Figure 6: X-ray TBS in the anterior-posterior projection of patient B., 5 years Diagnosis: "Pertes disease on the right, stage II", admission Catteral II, hypo function of MANPADS.

Figure 7: X-ray TBS in the anterior-posterior projection of the patient T. 4 years. Diagnosis: "Perthes' disease on the right, stage II", on admission Catteral II, destruction of MANPADS.
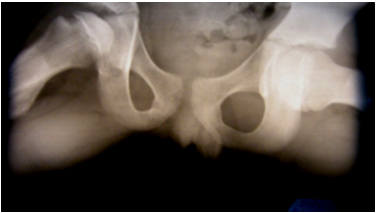
Figure 8: X-ray of TBS in the position of Lauenstein K., 10 years Diagnosis: "Disease Pertes right, II stage", when entering Herring and degeneration PSRBC.
Studying the CT-picture in all 65 patients, upon admission, the location, the magnitude of the prevalence of necrosis of the femoral head and its volume were determined. All 36 patients under 8 years of age reported that at the beginning of the disease it was located in the apical part of the femoral head, and then began to spread along the anterior-outer surface, occupying 6–9 sectors, and its volume was 560 – 982 mm3. The average volume of a healthy head at this age was 7250 – 7580 mm3. Whereas in 19 patients with stage III blcp the value of bone resorption was significantly higher. In 10 cases, it occupied 5 – 11 sectors, and the volume of osteonecrosis reached 3620 – 3800 mm3, and in 9 cases its spread to the posterior surface of the thigh led to a SCT picture of total defeat.
In 10 children over 8 years old necrosis in disease onset was localized in the outer surface of the epiphysis of the femur over PSRBC and vector distribution was different. He did not occupy any sector. The strength of the trabecular system in 46 children with stage II blcp decreased compared to healthy TBS (p < 001) by 100 units and amounted to 120 – 180 (+ Hu). In 19 patients with stage III of the disease, bone loss in the area of osteonecrosis was significantly greater and amounted to 110 – 50 (+ units HU) (p < 0.5). Analysis of laboratory parameters in 20 patients with blcp (10 children with II and 10 with III stages of blcp) revealed a significant increase in β-CCS Laps. In 10 children with stage II, it was 2.5 – 5.3, and in 10 studied its values in stage III exceeded 5.6 – 8.9 ng/ml (p < 001). The change in this indicator allows to determine the increase in bone resorption in patients with blcp.
However, it is necessary to pay attention to the fact that during the physiological acceleration of growth in children and adolescents, there is an increase in it at the age of 5 – 6 years, 11 – 12 years in girls and 13 – 14 years in boys. This process is usually associated with increased bone remodeling and increased skeletal mass in these age and sex intervals. The study of the level of biochemical parameters: total protein, creatinine, calcium-phosphorus relationship in 46 children with stage II of the disease did not reveal significant violations. Whereas in 15 patients in stage III, the level of ionized calcium significantly aspired to the upper limit of the norm (p < 001), and the level of inorganic phosphorus remained within the norm. Indicators of total protein and creatinine were also not violated.
Studying the results of clinical examination, x-ray, computer-topographic and laboratory parameters in 6 months after intra-articular administration, it was stated that the course of the disease in all 65 patients with blcp were not similar. In 31 children (47.7%) with stunting up to 8 years, pain in the groin area was stopped, and gait disturbance was not noted. The relative length of the lower limbs was the same. The difference in the circumference of the soft tissues of the thigh did not change, and the amplitude of active movements in both TBS was restored. The x-ray pattern corresponded to stage III of the disease. The degree of disintegration of the bone tissue took up 50% of the affected epiphysis and the match between Catterall I - II. Its depth did not affect the MANPADS.
It had the same height and width as on the opposite side. The zone of drug calcification was clearly expressed, with a uniform optical density. The contours were coarse, indicating the restoration of its functional activity. The height of the epiphysis was reduced, but it retained a spherical shape. The width and length of the femoral neck did not differ from the identical figures on the opposite side. According to the CT data, the volume of osteonecrosis was 2000 mm3, occupying 6 – 9 sectors (25%) and located on the anterior surface of the thigh. Bone density in the fracture zone was 200 – 250, and outside the affected part of the epiphysis increased to 370 – 410 (+ Hu). Parameter β-Cogs Laps was 0.6 – 0.8 ng/ml. Other laboratory parameters were within the physiological norm.
Whereas, 6 months after intra-articular injection of Osteoprotegerin in 34 children (52.3%) with II - III stage BLK clinical and x-ray, CT and laboratory tests were different. In the clinical picture, all 24 children (5 with stunting and 19 with normal development) were relieved of pain, while maintaining lameness. Shortening of the affected lower limb was 1.0 cm due to the absolute shortening of the thigh. Hypotrophy of the soft tissues of the thigh was 1.5 cm. Contracture in the affected TBS was formed by limiting the diversion of internal and external rotation of the thigh - 10°. X-ray picture of all the examined corresponded to the III stage of the disease. The amount of destruction in children with short stature increased to of II degree in between Catterall and rentgenograficheskoe indicators PSRBC was characterized by a decrease in its height and width.
Areas of preparative calcification preserved its vagueness, and had a non-uniform optical density. In patients with normal physical development, the value of osteonecrosis was equal to the III degree of Catterall, and the radiological signs of violation of MANPADS were determined by the unevenness of its height and the formation of "stellate" sclerosis. The change in anatomy provoked a disruption in its functioning, which led to the formation of an absolute shortening of the thigh. The height of the head was sharply reduced, but its sphericity is not lost. The femoral neck became shorter in length and wider in transverse size compared to healthy TBS.
Resizing is not triggered the symmetry breaking intertrochanteric line. Smooth lines Sadofieva and Shenton continued. The volume of the destroyed part of the femoral head was 3600 – 4900 mm3, occupying 5 – 11 sectors (75%). It spread from the outer to the entire inner part of the patient's epiphysis with the transition to the neck of the thigh. Topographic survey of MANPADS revealed a change only in its anterior portion in the Central part. The density of bone tissue in the osteonecrosis area was 100 – 150, and outside the affected part was twice as much - 330 – 390 (+ Hu units).
In 10 patients (15.4%) of older age with hypersthenic Constitution pain was not stopped, and lameness progressed. Shortening of the lower limb increased to 1.5 cm, due to the absolute shortening of the thigh. Hypotrophy of the soft tissues of the thigh and Shin increased to 2.0 cm of the thigh and 1.5 cm in the Shin. The increase in tone in the muscles of the pelvic girdle and surrounding TBS provoked a restriction of hip retraction by 20° and a deficit of rotational movements of 15°. X-ray all patients was consistent with Herring A. Rentgenografija PSRBC changed. Its height increased, and the contours and structure of the zone of drug calcification retained its unevenness and heterogeneity.
The height of the proximal epiphysis was disturbed only in its outer part, and the length of the femoral neck decreased sharply. These structural changes led to asymmetry of the intertrochanteric line 1.0 cm step-like course leading to decentration the line Sadofieva and changed smoothly-curved bending line of Shenton, which marked the beginning of the formation of the FAI. The volume of necrosis of the femoral head bone tissue was 1600 – 2300 mm3, occupying 3 – 5 sectors (25%). In the destroyed part of the epiphysis bone density was 200 – 250, and outside the affected it increased to 300 – 340 (+ units HU). Topographically visualized the location of the destruction of MANPADS. It was localized, as in the anterior portion of the lateral part in the frontal plane, as well as in the outer and posterior portions in the sagittal plane. Biochemical parameter corresponded to physiological norm (Figure 9, 10, 11).
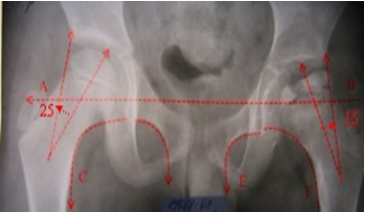
Figure 9: X-ray of TBS in the anterior-posterior projection of patient A., 6 years old Diagnosis: "Perthes' Disease on the left, stage III" Catteral III. The interbody line (A-B) is synchronous; the Shenton line (E-F) is interrupted by 5 mm; the lateralization angle is reduced by 10°.

Figure 10: CT picture of the prevalence of osteonecrosis of patient A., 6 years old Diagnosis: "pertes Disease on the left, stage III" Catteral III. Subtotal lesion of the femoral head.
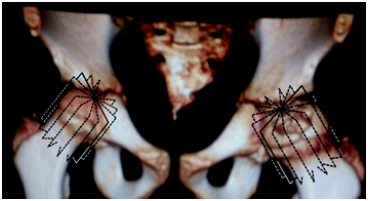
Figure 11: The picture SKT calculate the volume of osteonecrosis of the patient O., 6 years old Diagnosis: "Perthes Disease on the left, stage III" Catteral III. The volume of osteonecrosis is 3000 mm3
12 months after repeated x-ray examination, 31 children (group I) had no progression of intraosseous destruction of the proximal epiphysis. The relative length of the lower extremities was the same, the deficit of the volume of active movements was not revealed. The proximal epiphysis was significantly reduced in height, with a clear spherical outline. The MANPADS were traced throughout, its height and width being the same compared to the opposite side. Although, the dimensions of the femoral neck were broken, but the congruence of the articular surfaces of the TBS was preserved. According to the SCT, the volume of the destroyed part of the epiphysis was 1500 mm3, and the density in it was 200 (+ Hu).
The remaining 34 children and adolescents (II and III groups) retained the difference in the relative length of the lower extremities, increased hypotrophy of the soft tissues of the thigh. Contracture in the affected hips increased, the deficit of the abduction of the hip and internal rotation was 15°. X-ray pattern in 24 patients (group II) corresponded to stage III disease (Catterall III). The proximal epiphysis was separate fragments that were not connected with each other. Although its contour remained intermittent and sharply reduced in height, but The Shenton line remained smooth, and the Sadofieva line was rejected. PSRBC is practically not observed, and the neck of the femur sharply cropped and enlarged. The asymmetry of the interbody line reached 1.5 cm, which led to the formation of FAI.
The thickness and uniformity CHGBK preserved throughout. At the same time, the volume of osteonecrosis has not changed, and its sectorality has remained the same. Topographically detected an increase of the defect the destruction PSRBC. It already covered the entire front and middle portions, and its depth reached 2/3 of the cross-section of the femur. Bone density in the area of bone destruction was 150 – 180 (+ units HU), with a clear rim of the osteosclerosis zone throughout the destruction zone. In unaffected areas it was 390 – 450 (+ Hu units). Biochemical parameters remained within the physiological norm. An increase in the density of bone tissue of the femoral head in non-affected areas more than twice and the formation of the osteosclerosis zone along the entire length of the femoral neck may indicate the beginning of reparative bone regeneration.
Whereas, in 10 children and adolescents (group III) structural disorders in the proximal epiphysis continued to progress. The deterioration of the main static-dynamic parameters was clinically diagnosed. The relative length of the patient's lower limb became shorter by 1.5 - 2.0 cm, and hypotrophy of the soft tissues of the thigh by 2.5 cm. Restriction of movements in TBS increased. Deficiency of abduction and internal rotation of 25°. Analysis of x-ray parameters revealed the spread of bone necrosis to the sixth segment - Herring B. the Changes also affected the anatomy of MANPADS. It was extended in height, with uneven contours. The height of the proximal epiphysis was reduced and the neck shortened and enlarged. The spatial disturbance of the intervertebral line increased to 2 cm, which provoked the shift of the Sadofieva line to the outer part of the acetabulum in 6 patients.
The Shenton line had a step bend, more than 5 mm. FAI continued to progress, which led to the convergence of articular surfaces. The volume of osteonecrosis was 2500 – 3300 mm3, occupying 3 – 6 sectors (50%) of the outer part of the head. The average values of the volume of the proximal epiphysis of healthy TBS at this age ranged from 7620 – 8150 mm3. Bone density in the affected area decreased to 150 - 100 (+ Hu), and in the unchanged areas of the epiphysis increased 390 – 450 (+ Hu). Photo mechanically process resulted in compression not only CHGBK, but cartilage of the acetabulum. Height CHGBK in the contact area was reduced to 1 mm. The FAI is permanent. Topographically, there was a deepening of destruction in all planes and portions of the PZRBC to ½ of the cross-section of the femur. It gave us the right to re-periarticular the introduction of osteoblastoma (Figure 12, 13, 14).
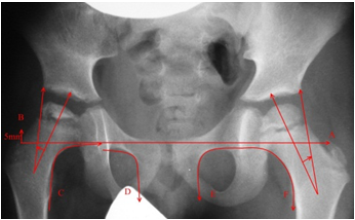
Figure 12: X-ray of TBS in the anterior-posterior projection of patient F., 7 years old Diagnosis: "Perthes' Disease on the right, stage III" Catteral III. Intertrochanteric line (A-b) step-like broken on the right by 5mm; Shenton's line (C-D) suspended for 5mm; the angle of lateralization is reduced by 10°; the FAI on the right is short-lived.
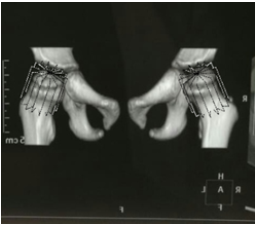
Figure 13: SCT picture of the volume of osteonecrosis of patient F., 7 years old Diagnosis: "Perthes Disease on the right, stage III" Catteral III. Subtotal lesion of the femoral head, the volume of osteonecrosis is 4500 mm3.

Figure 14: Radiograph of TBS in the anterior-posterior projection of the patient K., 11 years old Diagnosis: "Avascular necrosis of right hip, stage II" Hering B. Intertrochanteric line (A-b) step-like broken right at 15mm; Shenton's line (C-D) suspended for 10 mm.
Continuing the dynamic monitoring of all patients after 18 months from the beginning of treatment, it was stated that the rate of reparative regeneration was different. In children of group I in orthopedic status, while maintaining the same length of the lower limbs, there was no restriction of movements in TBS, the tone in the thigh muscles increased, and radio graphically there was a transition of stage III of the disease in IV. The contours PSRBC was moderately curved. The area of preparative calcification homogeneous. Positive dynamics of the beginning of remodeling of the femoral head shape and structure was revealed. The proximal epiphysis was a single structural conglomerate, it had a spherical shape, with a significant increase in its height. The CT scan also showed restoration of the femoral head structure. The volume of bone necrosis decreased to 1000 mm3, and bone density increased to 220 - 260 (+ Hu).
In patients of group II, the relative length of the lower extremities was the same, there were no restrictions on active movements in TBS. The x-ray image indicated that the structure of the proximal epiphysis corresponded to stage III blcp. X-ray anatomical parameters of MANPADS were characterized by non-uniformity of its height and width. Its shape was wedge-shaped, the course was straight, with V and A – shaped deformation and jagged contours. The zone of drug calcification was not homogeneous. However, bone regeneration was begun distinctly to manifest itself. The area of osteonecrosis was combined with foci of local osteosclerosis. Its location was most often recorded in the area of former trabecular fractures. The course of the intertwining line, Sadofieva and Shenton was smooth.
FAI was short-term and was liquidated in 6 months. Bone density in all areas was the same 390-450 (+ units HU). Due to the activation of bone regeneration, the volume of osteonecrosis and its sectorality began to decrease. The number of sectors decreased to three 6-9 (50%), and the volume of 2500-3000mm3. Topographically, the destruction of the anterior and middle portions of MANPADS was preserved. However, its depth was reduced to ½ the diameter of the femur and focused only in the Central part. The slowest regeneration process was recorded in group III patients. In the orthopedic status, the difference in the relative lengths of the lower extremities was preserved, due to the absolute shortening of the thigh by 1.5cm, hypotrophy of the soft tissues of the thigh and Shin.
Deficiency of abduction and 10°, and internal rotation to 15°. Radiologically, the extent of osteonecrosis was equal to Herring V. Anatomy PSRBC kept the typical radiological signs of degenerative changes. The shape and structure of the femoral head were not uniform due to the low bone density in the fracture zone of 180 (+ Hu) and virtually no change in the volume of osteonecrosis. Topographically, its version of destruction remained the same. Pathological contact between the articular surfaces led to their collision. Height CHGBK in the field of focused compression was equal to 1.0 mm, with the formation of V – defect (Figure 15, 16, 17).
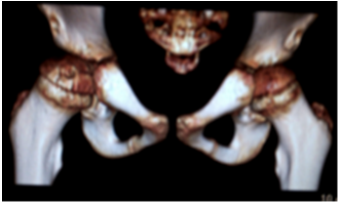
Figure 15: SCT picture of TBS patient G., 7 years old Diagnosis: "pertes Disease on the right, stage IV" Stulberg A.
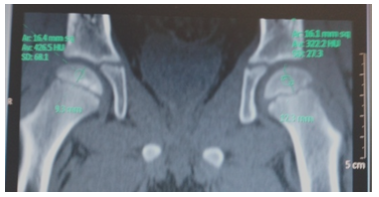
Figure 16: SCT picture of TBS patient G., 7 years old Diagnosis: "pertes Disease on the right, stage IV", bone density on the right increased to 260 units of Hounsfield.
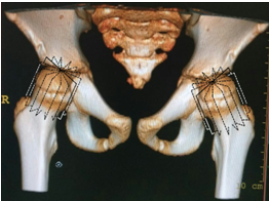
Figure 17: SKT picture of the TBS patient F., age 9 Diagnosis: "Perthes Disease on the left stage of the Exodus," Stulberg A.
After 24 months in group I patient’s orthopedic status has not changed. The transition of stage IV of the disease to the stage of outcome was determined radiologically. The architectonics of the trabecular system and the shape of the femoral head did not differ from the healthy Stulberg – A. the x-Ray analysis of the pzrbc anatomy revealed no significant abnormalities in comparison with the contralateral side. SCT showed the presence of a bone defect in the apical part of the femoral head with a volume less than 10 mm3. The density of both proximal epiphysis were the same.
No biochemical abnormalities were found. In children of group II in orthopedic status did not reveal a difference in static-dynamic indicators. Radiographically, the proximal epiphysis of the femur had a single structure, which corresponded to stage IV blcp, but its shape retained variability from spherical Stulberg – A (55%) to mushroom – B (45%). The contours PSRBC was krupnojacheistye that indicated the intensity of its growth. The amount of bone resorption was reduced to 1500-1700 mm3, and the bone strength was increased 300-350 (+ HU units). The number of osteonecrosis sectors decreased to two 6–7 (25%). Topographically, the process of destruction occupied the Central part of the anterior portion of the MANPADS.
Adolescents of group III showed positive dynamics in orthopedic status. Orthopedic shortening of the affected lower limb was equal to 1.0 cm, and wasting of the soft tissues of the thigh 1.5cm Deficiency of abduction - 5°, and internal rotation – 10°. The x-ray image retained a change in the shape of the proximal epiphysis (Herring In). X-ray anatomy of MANPADS has not changed. The beginning of reparative regeneration was traced in the femoral neck area in the form of bone tissue compaction with distinct local osteosclerosis. The strength of the rigid tissue in the area of osteonecrosis, according to SKT increased to 210 – 220 (+ Hu units). The FAI was stopped after 16 months, but in the outer part CHGBK remained V – defect. Topographically recorded the destruction of only the front portion PSRBC ½ of the width of the femoral neck.
After 30 months of dynamic follow-up, 55 (84.6%) children of groups I and II had no new orthopedic disorders. Radiographically, in 45 cases (81.8%), the spherical shape of the femoral head was registered, in 6 (10.9%) - fungal, and in 4 (7.3%) - "coxa magna". The shape of the head depended on the speed of recovery and synchronicity of functioning of portions of MANPADS. Topographically all portions PSRBC in 45 cases operated synchronously. In 6 cases, the anterior portion did not function fully, which led to the formation of a mushroom head. In 4 cases, an increase in the function of the Central part of the anterior and middle portions was found, which provoked hypertrophy of the femoral head.
The CT analysis showed the presence of a bone defect in the apical part of the femoral head with a volume of 20 – 25 mm3. Patients of group III showed a distinct positive clinical and radiological dynamics. The relative length of both lower limbs was the same. Wasting of the soft tissues of the hips was equal to 1.0cm. Deficit in internal rotation was 10°. The muscle tone of the pelvic girdle and the surrounding of TBS was recovered. The activity of reparative regeneration was accompanied by a decrease in the degree of osteonecrosis (Herring A). Rentgenologicheski PSRBC analysis showed restoration of the height and the uniformity of areas of preparative calcification. The structure of the PCOB did not maintain its uniformity, but the strength of bone tissue increased to 310 – 400 (+ Hu). Topographically CHGBK kept the V - defect. The destruction of the MANPADS focused only on the front of it.
After 36 months of follow-up, all 65 patients had the same relative length of lower limbs. In the Orthopaedic status in 6 Teens in the group III there remained a deficit of internal rotation of the hip 5°. The circumference of the soft tissues of the thigh was the same. In the x-ray picture in 55 (84.6%) children of groups I and II, the shape of the femoral head corresponded (Stulberg - A). In 5 adolescents of group III, the structure and density of the bone tissue of the PCOB did not differ from the contralateral side and corresponded to - Stulberg – B. Topographically remained a malfunction of the front portion PSRBC. In one case, the shape of the femoral head was equal to (Herring A). Its structure has not retained its homogeneity, V-defect CHGBK remained. In 40 months clinical, radiographic and CT studies showed the restoration of basic static and dynamic characteristics, shape and structure PCB and density of the femoral head have all 10 adolescents matched - Stulberg – Topographically A. all portions PSRBC operated synchronously. Thickness CHGBK was restored.
When discussing the obtained results we came to the conclusion that the rate of reparative regeneration in children with BLK depended on the patient's age, physical development, the value of the volume of osteonecrosis and violations PSRBC. Osteoprotegerin needs to take a leading place among the pharmacological agents in children with blcp [3, 11, 13 and 15]. However, the oral and intravenous route of administration to the focus of bone necrosis is questionable. The first for the duration of transportation, and the second due to severe complications in the somatic status of the child. Reduction of osteonecrosis volume and increase of bone tissue density can be considered as indisputable evidence of reparative regeneration [12].
Hemodynamic and rheological disorders in TBS vessels are caused either by a decrease in the tone of the vascular wall or by stenosis of the arteries surrounding the femoral neck [2, 4 and 6]. Angioprotectors and venotonics should be used to effectively support reparative regeneration [6, 8-10 and 16]. The state of MANPADS is subject to mandatory x-ray and CT analysis on the basis that its structure is disturbed and functional activity is sharply inhibited [17-18]. The recovery of the spherical shape of the femoral head depends on the activity and synchronicity of the functioning portions PSRBC. Bone regeneration of the femoral head in children with different physical development proceeds differently.
Myelodysplastic disorders cause changes not only in vascular tone, but also in pelvic girdle and thigh muscles [6]. Discordance muscles of the pelvic girdle and thighs, forcing the articular surfaces of TBS first approach and soderjatsya, and that forms the FAI. Its pathomechanical process leads not only to a decrease in the width of the joint gap TBS, but also to a change in the congruence of joint surfaces. Violation of the spatial geometry of the PCOB causes lateralization, and then the saddle-shaped deformation of the femoral head. The formation of multi-plane deformations of the PCOB forces the orthopedist to perform complex reconstructive surgery [8, 12].
Conclusion
Thus, one of the main mechanism of stimulation of reparative regeneration of bone tissue in patients with BLK can be considered the use of intra-articular and periarticular the introduction of osteoprotective. His most favorable outcome recorded in patients under 8 years of age, low physical development, the volume of osteonecrosis to 50% and PSRBS in a state of hypo function in 12-18 month (Stulberg). In children with normal physical development the main reason for speed reduction of osteoregenerative was the increasing depth of osteonecrosis to 75%, the destructive option of functioning PSRBC and introduction into the hearth of destruction of its separate portions.
Restoration of normal x-ray anatomy and functioning of MANPADS occurred after 18-24 months. The longest process of reparative regeneration was observed in adolescents with growth above average. The shape and structure of the femoral head and the functional activity PSRBC recovered within 24 to 30 months. The formation of FAI leads to gross violations of the shape of the femoral head. Modern orthopedics of childhood and adolescence does not have methods of gene therapy. Therefore, at the moment the main ally of the reparative regeneration, it is necessary to consider the use of osteodensitometry drugs that help to stop the progression of this disease.
References
- Su P., et al. “A histological and ultrastructural study of femoral head cartilage in a new type II collagenopathy”. International Orthopaedics 34.8 (2010):1333-1339.
- Reiser M., et al. Kostno-mushechnay sistema Direct Diagnosis in Radiology. Musculoskeletal imaging. Moscow: MED press-inform 2011. (In Russ).
- Тихоненко Т.И. Оценка остеогенезстимулирующих методов при лечении болезни Легг-Кальве-Пертеса у детей: Дис. ...канд. мед. наук. – Москва; 2011. [Ocenka osteogenezstimulirushih metodov pri bolezni Legg-Kalve-Pertesa. [Dissertation] Moskva; 2011 (In Russ).]
- Lobov I.L., et al. “Analysis of the physical growth and markers of connective tissue dysplasia in patients with Perthes disease”. Pediatric Traumatology, Orthopaedics and Reconstructive Surgery 6.2 (2018): 12-21.
- Brech GC and Guarnieiro R. “Evaluation of physiotherapy in the treatment of Legg-Calve-Perthes disease”. Clinics 61.6 (2006): 521 – 528.
- Барсуков Д.Б. Болезнь Пертеса //Педиатрия. – 2009. – №3. – С. 24 — 30. [Barsukov D.B. Perthes disease Pediatria 2009; (3): 24 — 30. (In Russ).]
- Terjese T., et al. “The natural history of Perthes' disease”. Acta Orthopaedica81.6 (2010): 708 – 714.
- Куликов Н.Н. Оптимизация хирургической помощи детям с болезнью Пертеса: Дис. ...док. мед. наук. – Москва; 2010. [Optimizacia hirurgicheskoy pomoshi detiam c bolezni Pertesa. [Dissertation] Moskva; 2010 (In Russ).]
- Захарова Н.В. Применение мексидола в комплексном лечении болезни Легга-Кальве-Пертеса: Дис. ...канд. мед. наук. – Якутск; 2012. [Primenenie mecsidola v kompleksnom leshenii bolezni Legg-Kalve-Pertesa. [Dissertation] Yakutsk; 2012 (In Russ).]
- Таусиф Раза Диагностика и лечение болезни Легг - Кальве – Пертеса: Дис. ...канд. мед. наук. – Иваново; 2005. [Diagnostica i lechenie bolezni Legg-Kalve-Pertesa. [Dissertation] Ivanovo; 2005 (In Russ).]
- Kozcvnicov OV., et al. “Kompleksnay medicamentoznay terapiy narusheniy calci-fosfornogo obmena u detey s zabolevaniymi oporno-dvigatelnogo apparata”. In: Proceedings of the Russian pediatrics orthopedics congress, Topical issues of traumatology and orthopedics children's age (2009): 334-335.
- Лысиков В.А Хирургическое лечение болезни Легг-Кальве-Пертеса: Дис. ...канд. мед. наук. - Москва; 2017. [Hirurgichskoe leshenie bolezni Legg-Kalve-Pertesa. [Dissertation] Moskva; 2017 (In Russ).]
- Johannesen J., et al. “Systemic effects of zoledronic acid in children with traumatic femoral head avascular necrosis and Legg-Calve-Perthes disease”. Bone 45.5 (2009): 898-902.
- Kim H.K. “Pathophysiology and new strategies for the treatment of Legg ― Calvé ― Perthes disease”. Journal of Bone and Joint Surgery 94.7 (2012): 659-699.
- Akhtyamov IF., et al. “History of development of non-operative treatment Legg-Calve-Perthes disease”. Practical Medicine4 ( 2016): 38-43.
- Фишкин В.И., Дудинов В.Н. Ранняя диагностика и лечение остеохондропатий головки бедренной кости. В кн.: Метод. рекоменд. Иваново; 1982. с. 39. [Fishkin V.I., Dudinov V.N. Rania diagnostica i leshenie osteochondropatii golovki bedrennoy costi. Ivanovo: 1982. (In Russ).]
- Садофьева В.И. Нормальная рентгеноанатомия костно-суставной системы детей. – Ленинград, 1990. [Sadof'eva V. I. Normalnay rentgenoanatomia costno-sustavnoy sistemu y detey. Leningrad: 1990. (In Russ).]
- Teplen'ky MP., et al. DYNAMICS OF WIDTH OF PROXIMAL FEMORAL GROWING ZONE IN PATIENTS WITH PERTHES DISEASE AFTER SURGICAL TREATMENT. Traumatology and Orthopedics of Russia 3 (2014): 60-68.
- Steppacher SD., et al. “Femoral morphology differs between deficient and excessive acetabular coverage”. Clinical Orthopaedics and Related Research 466.4 (2008): 782–790.
- Патент РФ на изобретение №2487682/20.07.13. Бюл. № 20. Лобов И.Л. Способ лечения некроза головки бедренной кости. [Patent RUS № 2487682/20.07.13. Byul. № 20. Lobov I.L. Sposob lechenia necroza golovci bedrennoy costi. (In Russ).
Citation:
IL Lobov., et al. “Improving the Effectiveness of Reparative Regeneration in Children and Adolescents with the Disease Legg – Calve – Perthes”. Orthopaedic Surgery and Traumatology 2.5 (2019): 417-432.
Copyright: © 2019 IL Lobov., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.