Research Article
Volume 2 Issue 5 - 2019
Surgical Management of Giant Cell Tumour of Tendon Sheath (GCT-TS) of Hands – an Institutional Experience
1Professor & Unit Chief, Department of Orthopaedics, JJM Medical College, Davangere, Karnataka, India
2Junior Resident Department of Orthopaedics, JJM Medical College, Davangere, Karnataka, India
2Junior Resident Department of Orthopaedics, JJM Medical College, Davangere, Karnataka, India
*Corresponding Author: Madhan Jeyaraman, Junior Resident Department of Orthopaedics, JJM Medical College, Davangere, Karnataka, India.
Received: January 14, 2019; Published: January 29, 2019
Abstract
Introduction: Swellings of the hand were most commonly encountered in the general practise with different diagnosis. For all such swellings, the differential diagnosis of ganglion, giant cell tumour of tendon sheath, osteoarthritic nodules, rheumatoid nodules, tophaceous gout, epidermoid cyst and lipoma have been to be considered. Giant cell tumour of tendon sheath present as second most common tumourous lesions next to ganglion cyst. This article aims at the management of giant cell tumour of tendon sheath.
Objectives: To evaluate the efficacy, functional outcome and recurrence of surgical management of giant cell tumour of tendon sheath.
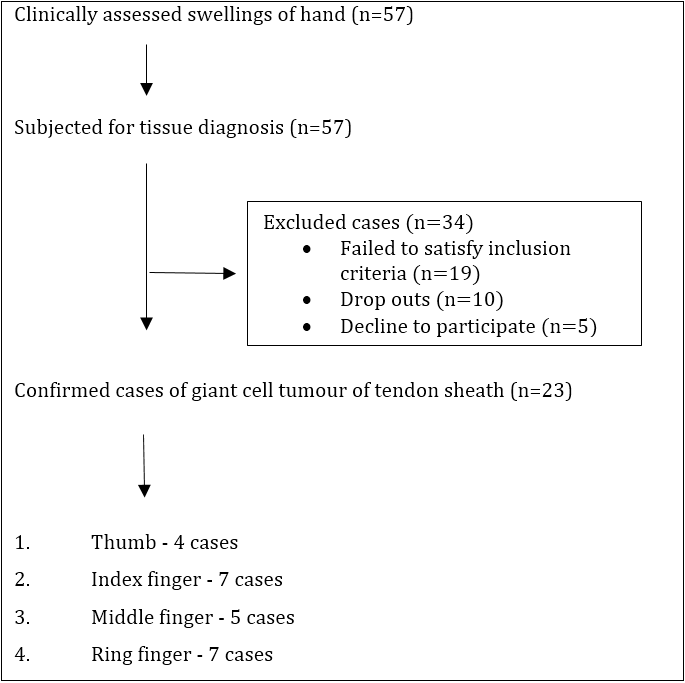
Methods: A total of 57 cases of hand swellings have been encountered from August 2016 to July 2018. After confirmation of tissue diagnosis, 23 cases enrolled in the study and have been treated with an excision biopsy of the tumourous lesion in toto with chemical cauterisation. The cases were followed up post procedure at the end of 1st, 3rd, 6th and 12th month for complications and the data were analysed statistically.
Results: Out of 57 cases of hand swellings, 23 cases have been proven cytopathologically as giant cell tumour of tendon sheath of flexor digitorum superficialis and flexor digitorum profundus. Out of 23 cases, 9 cases were males and 14 cases were females. The lesions were present in thumb 4 cases, index finger 7 cases, middle finger 5 cases and ring finger 7 cases. All 23 cases were treated by excisional biopsy of lesion and chemical cauterisation with hydrogen peroxide sponging under loco-regional anaesthesia. The specimens were sent to histopathological studies. No adverse reactions and recurrence of tumours were noted in the study participants after 1 year of follow up.
Conclusion: The differential diagnosis of swellings of the hand should be addressed off. The surgical excision of tumourous lesions in toto with hydrogen peroxide sponging remain the gold standard treatment of giant cell tumour of tendon sheath. A strict surveillance have to be done for recurrence of tumourous lesions.
Keywords: Giant cell tumour; Tendon sheath; Osteoclastic giant cell; Cauterisation
Introduction
Swellings of the hand were most commonly encountered in the general practise with different diagnosis. For all such swellings, the differential diagnosis of ganglion, giant cell tumour of tendon sheath, osteoarthritic nodules, rheumatoid nodules, tophaceous gout, epidermoid cyst and lipoma have been to be considered. Giant cell tumour of tendon sheath present as second most common tumourous lesions next to ganglion cyst [1].
GCT-TS has an indolent course of slow growing, painless benign tumourous lesion of soft tissues. It affects individuals between 3rd to 5th decades of life and is more commonly seen in women than men [2]. The intrinsic biology of giant cell tumour of tendon sheath is poorly understood. There is no specific protocol for management of GCT-TS. Despite benign, GCT-TS has a malignant potential and to metastasize. Surgical excision in toto with or without post radiotherapy is the choice of management of GCT-TS. The most common problem encountered during follow up period is the recurrence (45%) [3]. The recurrence is due to the presence of satellite nodular lesions, improper excision due to the presence of neurovascular bundles and bony involvement.
This article aims in the management of GCT-TS with excision biopsy in to and chemical cauterization with hydrogen peroxide. A strict surveillance has been attributed for recurrence of tumorous lesions in the follow up period.
Materials and Methods
- Health care setup – Tertiary care hospital
- Setting – JJM Medical College, Davangere, Karnataka.
- Duration of the study – August 2015 to July 2018
- Type of the study – Prospective cohort study
- Level of evidence - Level IV
- Sample size – 57
- Selection of cases – 57 cases of swelling of the hands were clinically identified. After tissue diagnosis of tumourous lesions, 23 cases were proven as giant cell tumour of tendon sheath. These 23 cases were taken up for this study who were treated with excisional biopsy of lesion and chemical cauterisation with hydrogen peroxide sponging under loco-regional anaesthesia and followed up as per our study protocol.
- Follow up – At the end of 1st, 3rd, 6th and 12th months
Inclusion criteria
- Patients with confirmed tissue diagnosis of giant cell tumour of tendon sheath
- Patients who gave consent for surgical treatment as per our protocol
- Regular follow up visits in the out-patient department
Exclusion criteria
- Patients with confirmed tissue diagnosis other than giant cell tumour of tendon sheath
- Patients with local infection at the site of the procedure, HIV, Hepatitis B or C, septicaemia and other systemic disorders
- Patients refusal for surgical treatment as per our protocol
After getting IEC clearance from the institute and informed written consent from the patients enrolled in our study, they were subjected for thorough clinical examination and to investigate the duration of the disease and the nature of management taken prior to the proposed surgical management of tumourous lesions. The baseline investigations such as complete hemogram, ESR, CRP, renal function tests, serum uric acid, random blood glucose, serological testing for HIV 1 & 2 and HbsAg and radiographic analysis of pathological sites were analysed. Radiograph of right hand in AP and lateral view revealed soft tissue shadow over DIP of ring finger without any bony involvement (as shown in Figure 4).
All the cases were sent for fine needle aspiration cytology for confirmation of GCT-TS. Cytopathology (FNAC) report of swelling over distal phalanx of right ring finger shows scatted plump spindle cells admixed with numerous osteoclast like giant cells. The scattered spindle cells have moderate amount of cytoplasm and oval pale nuclei without any granuloma formation (as shown in Figure 5). The cases with confirmed cytopathological diagnosis of GCT-TS were subjected for surgical management.
Pre procedural precautions: The cases were given test dose of lignocaine in the flexor aspect of forearm to check the lignocaine sensitivity.
Surgical technique: All the cases were operated by same surgeon. All cases underwent excisional biopsy (in toto excision with margin of normal tissue) of lesion over tendons of flexor digitorum superficialis and flexor digitorum profundus and chemical cauterisation with hydrogen peroxide sponging under loco-regional anaesthesia with uneventful postoperative events (as shown in Figure 6 and Figure 7). Intraoperatively, a total of 13 cases were single nodule surrounded by thick pseudo capsule, 3 cases with single nodule within a thin capsule and 7 cases were multi-lobulated surrounded by a common capsule.
Post procedural care: A course of antibiotics were given for all the cases and were followed up for functional outcome of surgical management of tumourous lesions and complications at the end of 1st, 3rd, 6th and 12th month.
Histopathology report of the excisional biopsy
- Grossly, the excisional biopsy specimen measured around 2-3 cm, well circumscribed and lobulated (as shown in Figure 8).
- Cut specimen appear yellow to tan areas due to the presence of xanthoma cells and hemosiderin pigments.
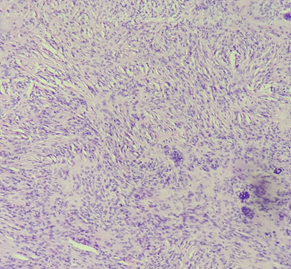
- Histopathology of the excisional biopsy showed a well-encapsulated tumour composed of abundant mononuclear cells and osteoclast type of giant cells along with thick fibrous septa running through the tumour (as shown in figure 9, 10a and 10b). Foamy cells, hemosiderin-laden macrophages, and cholesterol clefts were also seen which confirm the diagnosis of giant cell tumour of tendon sheath.
Results
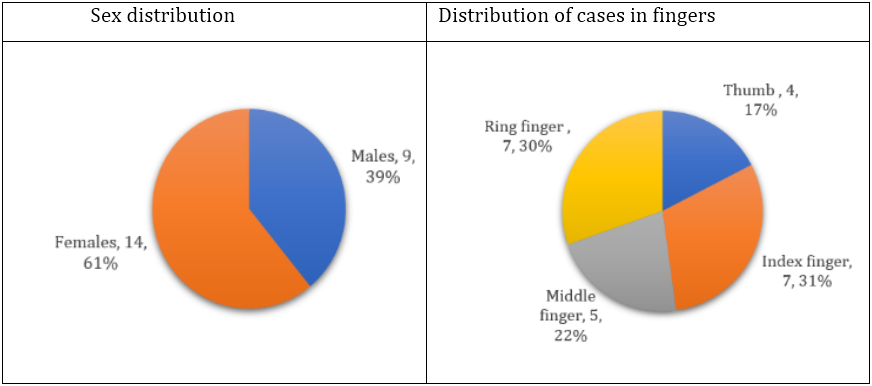
The data obtained from the participants of the study were subjected to survival test and the following results are obtained. Out of 57 cases of hand swellings, 23 cases have been proven cytopathologically as giant cell tumour of tendon sheath. Out of 23 cases, 9 cases (39.13%) were males and 14 cases (60.86%) were females. All patients were ranging between 32 to 56 years with mean being 41.73 years. The lesions were present in thumb 4 cases (17.39%), index finger 7 cases (30.43%), middle finger 5 cases (21.73%) and ring finger 7 cases (30.43%).
| Location | Thumb | Index finger | Middle finger | Ring finger |
| Proximal phalanx | 3 | 2 | 1 | 2 |
| Middle phalanx | - | 3 | 1 | 1 |
| Distal phalanx | 1 | 2 | 3 | 4 |
| Total | 4 | 7 | 5 | 7 |
Table 1: Distribution of GCT-TS among fingers.
All 23 cases were treated by excisional biopsy of lesion over tendons of flexor digitorum superficialis and flexor digitorum profundus
and chemical cauterisation with hydrogen peroxide sponging under loco-regional anaesthesia. The specimens were sent to histopathological studies. No adverse reactions and recurrence of tumours were noted in the study participants after 1 year of follow up.

Figure 4: X ray of right hand – AP & Lateral view showing soft tissue shadow over DIP of ring finger without any bony involvement.
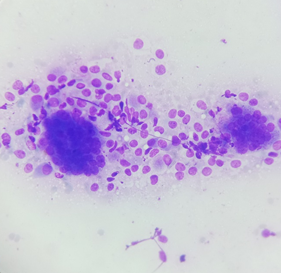
Figure 5: Giemsa stained FNAC (40x) showing osteoclast like giant cells admixed with mononuclear cells.
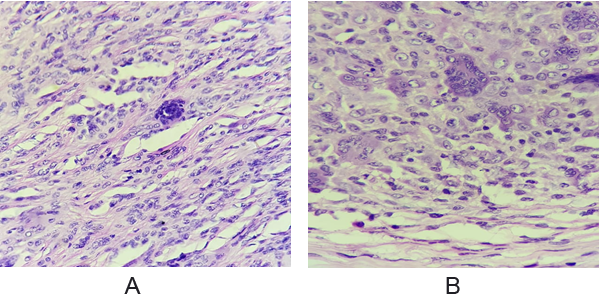
Figure 10a and 10b: HPE (40x) showing abundant mononuclear cells and osteoclast type of giant cells along with thick fibrous septa suggestive of giant cell tumour of tendon sheath.
Discussion
Giant cell tumour of tendon sheath is also called as benign synovioma, localized nodular tenosynovitis, tenosynovial GCT, synovial fibrous histocytoma, histiocytic GCT, pigmented villonodular synovitis, xanthomatous GCT, synovial xanthoma, xanthogranuloma, xanthosarcoma, fibrous xanthoma, Adenofibroma, fibro hemosideric sarcoma, giant-cell fibro haemangioma, and localized nodular synovitis [4].
The intrinsic biology of the tumour is poorly understood. Jaffe et al suggested GCTTS as a tenosynovitis, a non-neoplastic reaction [5]. Vogrincic., et al. emphasised the presence of polyclonal cells in the lesion by PCR assay for methylation of the X-linked human gene [6]. Using FISH probes, Nilsson., et al. detected the breakpoints localized to 1p13, often partnered with 2q35, which further proves 1p13 breakpoint appears to have a major oncopathological role in GCT-TS [7]. Increased expression of CSF-R1 by autocrine mechanism in cells of the lesion suggests GCT-TS as a neoplastic lesion. GCT-TS has a tumour landscaping mechanism in which it contains minor component of neoplastic cells and major component of inflammatory cells which are recruited by CSF-1 produced by neoplastic cells [8].
The giant cell tumour of the tendon sheath (GCT-TS) has a major indolent course with slow growing, painless, well circumscribed tumourous lesions of soft tissues. It affects more often women, with the mean age ranged from 30 to 50 years [2]. In our case series, females outweigh males in the ratio of 2:1. GCT-TS most commonly occurs in flexor aspect of hands, ankles, toes and knees. The most frequent tumour location is index finger, thumb, middle finger, ring finger and little finger [3]. In our study, the lesions were more common in index finger 7 cases (30.43%) and ring finger 7 cases (30.43%).
GCTTS are classified into localized nodular type (common in hand) and diffuse type (common in joints) by Byers [9]. Al-Qattan classified GCT-TS as Type-I, single tumour which is round or multilobulated, and Type-II, where there are two or more distinct tumours which are not joined [10]. In our study, 16 lesions (69.56%) were of single & nodular and 7 lesions (30.43%) were of multinodular in nature.
The MRI of giant cell tumour of tendon sheath are highly characteristic which show isointense to hypointense on T1 and hypointense on T2 weighted images. The characteristic low signal on T1 and T2 weighted images is attributed to the paramagnetic effect of hemosiderin and the abundant collagenous stroma [9,10].
The gross morphological features of GCT-TS are well-circumscribed lobulated or multinodular, greyish yellow to tan, encapsulated mass with varying degrees of hyalinization. Histopathologically, the cellular infiltrate is constituted by macrophage-like mononuclear cells, osteoclast-like giant cells, and xanthomatous cells. Hemosiderin-laden macrophages and cholesterol clefts are also seen. Histological aspects of cellularity and mitosis does not affect the prognosis of cancer [11-13].
Surgical management remains the gold standard treatment of GCT-TS. GCT-TS is reportedly known for its local rate of recurrence of up to 45% after excision. The factors predictive of recurrence are pressure erosion on radiographs, location at the interphalangeal joint, presence of degenerative joint disease and incompletely excision which were concluded by Reilly., et al. and Grover., et al. [9, 14] Kitagawa., et al. and Lowyck., et al. did not find significant correlation of recurrence with the above mentioned factors [15,16]. Williams., et al. reported that type-II tumours have been associated with a higher recurrence rate compared to type-I tumours, due to an undetected satellite lesion and subsequent incomplete excision [17]. In our study, all cases were operated with in toto excision of tumourous lesion over tendons of flexor digitorum superficialis and flexor digitorum profundus with chemical cauterization. There were no recurrence of lesions in the follow up period.
Adjuvant radiotherapy is recommended if there is a high risk of recurrence or incomplete excision of a histologically aggressive tumour with bony involvement. GCT-TS has the potential of turning into a malignant lesion, but it rarely metastasize. Kotwal., et al. recommended 20 Gy in daily divided doses of 2 Gy as postoperative radiotherapy in view of incomplete excision, presence of mitotic figures and bone involvement [18]. In our study, we didn’t institute postoperative radiotherapy to prevent recurrences.
The differential diagnosis remains foreign body granuloma, necrobiotic granuloma, tendinous xanthoma, infection, ganglion cyst, lipoma, knuckle pad, epithelial sarcoma and epitheloid formation.
Conclusion
Nevertheless, GCT-TS should not be eliminated from the index of suspicion in nodular swellings of the hand. Giant cell tumour of the tendon sheath is a rare, benign tumour of hand with a malignant potential to metastasize. The cytopathological diagnosis has to be confirmed before management which guides the surgeon to decide the modality of management. The basic aim of management should be early diagnosis with operative excision along with chemical cauterization to prevent recurrences.
References
- Darwish FM and Haddad WH. “Giant cell tumour of tendon sheath: experience with 52 cases”. Singapore Medical Journal 49.11(2008): 879-882.
- Uriburu IJF and Levy VD. “Intraosseous growth of giant cell tumors of the tendon sheath (localized nodular tenosynovitis) of the digits: report of 15 cases”. Journal of Hand Surgery 23.4 (1998): 732-736.
- Suresh SS and Zaki H. “Giant cell tumor of tendon sheath: case series and review of literature”. Journal of Hand and Microsurgery 2.2 (2010): 67-71.
- Powdhan HP and Madhan Jeyaraman. “GCT Lesion of Tendon Sheath of Finger in Pediatric Age Group - A Rare Case Report”. International Journal of current Medical and Applied sciences 19.3 (2018): 83-85.
- Jaffe H., et al. “Pigmented villonodular synovitis, bursitis and tenosynovitis”. Archives of Pathology 31 (1941): 731-765.
- Vogrincic GS., et al. “Giant cell tumor of tendon sheath is a polyclonal cellular proliferation”. Human Pathology 28.7 (1997): 815-819.
- Nilsson M., et al. “Molecular cytogenetic mapping of recurrent chromosomal breakpoints in tenosynovial giant cell tumors”. Virchows Archiv 441.5 (2002): 475-480.
- West RB., et al. “A landscape effect in tenosynovial giant-cell tumor from activation of CSF1 expression by a translocation in a minority of tumor cells”. Proceedings of the National Academy of Sciences of the United States of America 103.3 (2006): 690-695.
- Reilly KE., et al. “Recurrent giant cell tumors of the tendon sheath”. Journal of Hand Surgery 24 (1999): 1298-1302.
- Al-Qattan M. “Giant cell tumors of tendon sheath: classification and recurrence rate”. Journal of Hand Surgery 26.1 (2001): 72-75.
- Liu PT. “Radiological reasoning: acutely painful swollen finger”. American Journal of Roentgenology188 (2007): A13-S17.
- Rodrigues C., et al. “Giant cell tumor of the tendon sheath: a retrospective study of 28 cases”. Journal of Surgical Oncology 68 (1998):100- 103.
- David R Lucas. “Tenosynovial Giant Cell Tumor: Case Report and Review”. Archives of Pathology & Laboratory Medicine 136.8 (2012): 901-906.
- Grover R., et al. “Measurement of invasive potential provides an accurate prognostic marker for giant cell tumor of tendon sheath”. Journal of Hand Surgery 23 (1998): 728-731.
- Kitagawa Y., et al. “The effect of cellular proliferative activity on recurrence and local tumour extent of localized giant cell tumour of tendon sheath”. Journal of Hand Surgery 29.6 (2004):604-607.
- Lowyck H and De Smet L. “Recurrence rate of giant cell tumors of the tendon sheath”. European Journal of Plastic Surgery 28.6 (2006): 385-388.
- Williams J., et al. “Recurrence of giant cell tumors in the hand: a prospective study”. Journal of Hand Surgery 35.3 (2010): 451-456.
- Kotwal PP., et al. “Giant cell tumour of the tendon sheath- is radiotherapy indicated to prevent recurrence after surgery?” Journal of Bone and Joint Surgery 82.4 (2000): 571-573.
Citation:
Madhan Jeyaraman., et al. “Surgical Management of Giant Cell Tumour of Tendon Sheath (GCT-TS) of Hands – an Institutional Experience”. Orthopaedic Surgery and Traumatology 2.5 (2019): 396-404.
Copyright: © 2019 Madhan Jeyaraman., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.







































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.