Research Article
Volume 2 Issue 1 - 2018
Effects of Percutaneous Laser Disc Decompression (PLDD) on Clinical Outcome of Teared Vs Intact Protruded Intervertebral Discs: A Prospective Cohort Study
1Associate Professor of Anesthesiology & Pain management, Program Director of Pain fellowship, Department of Anesthesioloy & Pain Medicine, Shahid-beheshti University of Medical Sciences, Tehran, Iran
2Assistant Professor of Anesthesiology & Pain management, Department of Anesthesiology & Pain Medicine, Shahid-beheshti University of Medical Sciences, Tehran, Iran
3Pain Medicine Fellow, Department of Anesthesiology & Pain Medicine, Shahid-beheshti University of Medical Sciences, Tehran, Iran
2Assistant Professor of Anesthesiology & Pain management, Department of Anesthesiology & Pain Medicine, Shahid-beheshti University of Medical Sciences, Tehran, Iran
3Pain Medicine Fellow, Department of Anesthesiology & Pain Medicine, Shahid-beheshti University of Medical Sciences, Tehran, Iran
*Corresponding Author: Seyed Mohammdareza Haji Seyyed Abootorabi MD, Department of Anesthesiology & Pain Medicine, Shahid-beheshti University of Medical Sciences, Velenjak, Tehran, Iran.
Received: January 31, 2018; Published: March 15, 2018
Abstract
Background and Aims: Minimally invasive procedures, such as percutaneous laser disc decompression (PLDD), have been performed to minimize procedure related muscle and ligament injury. The present study aims to evaluate the efficacy and compare the clinical outcomes of PLDD procedure on teared VS intact protruded intervertebral lumbar discs in symptomatic patients in a 6 months period using PLDD as the only treatment modality.
Materials and Methods: Sixty patients with central and parenteral disc protrusion who met the inclusion criteria participated in the study. Patients were divided into two groups: with and without tearing, and then all underwent PLDD procedure. Patients were followed for 4 weeks, 6 weeks, 4 months and 6 months, and pain score based on VAS and function based on ODI were assessed. Data analysis was done by SPSS software and p-value of less than 0.05 was considered to be significant.
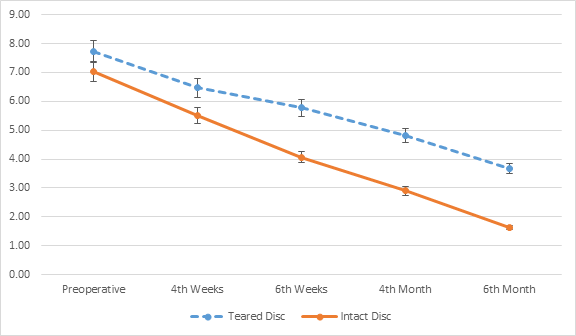
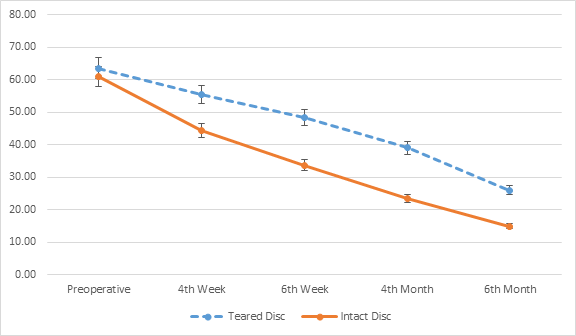
Results: The mean score of pain in all four postoperative follow-up stages was significantly lower in the intact disc group. Pain score was significantly decreased in patients with intact discs as compared to patients with disc tearing (p < 0.0001). Mean disability score based on ODI was significantly lower in all four postoperative follow-ups in the intact disc group. Disability score was also significantly reduced in patients with intact discs as compared to patients with teared disc (p < 0.0001).
Conclusion: PLDD showed more benefits on recovery of function and pain relief in patients with intact intervertebral herniated discs, compare to teared discs. We believe that early diagnosis and proper treatment in case of disc herniation provide a good chance for rapid alleviation. This result should be considered in patients' treatment protocol and planning, in order to obtain the best outcome.
Keywords: Discectomy; Percutaneous; Intervertebral disc displacement; Intervertebral disc disease; Pain measurement; Disability evaluation; Function recovery; Treatment outcome
Introduction
Lumbar disc herniation is among the most common causes of lower-back pain and its management has a wide-ranging variable modalities [1]. Patients are commonly treated in primary care, but a small proportion is referred to secondary care and may eventually undergo surgery when a related symptom continues for at least 6 weeks [2]. Conservative treatment is primarily aimed at pain reduction, by either analgesics or decreasing pressure on the nerve root without a conventional surgery [3]. Minimally invasive procedures, such as percutaneous laser disc decompression (PLDD), have been recently introduced and performed to minimize procedure related muscle and ligament injury [4]. Percutaneous laser disc decompression. (PLDD) is a possible alternative treatment for herniated lumbar disc disease. PLDD uses laser energy to vaporize a small volume of the nucleus pulpous, which reduces the pressure between the nucleus pulpous and the peridiscal tissue. This pressure loss induces retraction of the herniation away from the nerve root, thus reducing nerve root compression [5].
First proposed by Choy., et al. in 1984, this concept was validated by 2 years of in vitro experiments. Since the time the procedure was applied to large series of human patients and FDA approval was given to this procedure, quite a lot of studies have been published and showed the safety and potential benefits of PLDD, however the majority of the studies considered extrusion or sequestered disc herniation as exclusion criteria (5&6). Therefore, few studies have addressed the treatment of teared lumbar disc herniation by PLDD.
To date, no study has been performed in Iran to compare the efficacy and clinical outcomes of this procedure on teared VS intact protruded discs. The present study aims to evaluate the efficacy and compare the clinical outcomes of PLDD procedure on teared VS intact protruded intervertebral lumbar discs in 60 symptomatic patients in a 6 months period using PLDD as the only treatment modality.
Materials and Methods
This prospective cohort study was designed and conducted in Akhtar and Imam-Hussein academic hospitals (Tehran, Iran), during March –December 2017. The study was approved by ethics committee of Shahid-beheshti University of medical sciences under the registration number: IRSBMUREC1396124 and signed Informed consent was obtained from all the study participants. Study population was all patients presenting at pain management departments of mentioned academic hospitals during March-June 2017, whose lumbar intervertebral disc protrusions were confirmed by MRI and were candidate to undergo PLDD procedure.
Inclusion criteria included patients aged between 15-70 years, single-level central or paracentral lumbar intervertebral disc protrusion (either teared or intact) causing radiculopathy with no response to conservative therapy during past 6 weeks and Positive Lasegue test.
Patients with local or systemic infections; more than 50% loss of vertebral height; spinal canal stenosis; segmental instability or spondylolisthesis at the index level; neoplastic diseases; coagulopathy; apparent mental disorders; or history of previous surgery at the index level; pregnancy (regarding female patients) were excluded from the study.
Sample size was determined to 60, using comparison of two means formula and the following parameters from previous similar studies:
β = 80% → Z 1-β = 0.84
α = 0.05 → Z 1-α/2 =1.96
µ1 = mean VAS in tearing group: 3.31
S1 = 0.56
µ2 = mean VAS in non-tearing group: 3.75
S2 = 0.68
Sampling was performed by census method.
β = 80% → Z 1-β = 0.84
α = 0.05 → Z 1-α/2 =1.96
µ1 = mean VAS in tearing group: 3.31
S1 = 0.56
µ2 = mean VAS in non-tearing group: 3.75
S2 = 0.68
Sampling was performed by census method.
Patients were allocated to two groups of 30 according to disc status (teared or intact). History, demographic and baseline variables (back pain history, family history, co-morbidity, patient’s disability, weight and height, pain, and extent of protrusion based on preoperative MRI scan) were recorded in their profile by the main researcher and an appointment is made for 2 days later.
On the planned date, PLDD procedure was performed in a sterile operating room. The patient will be instructed to take a prone position on the surgical operation bed with a cushion under the lower abdomen to reduce lumbar lordosis. After placing sterile drapes, the level of treatment is identified by C-arm fluoroscopy. The needle entry point is anesthetized by local lidocaine injection, no deeper than the facet joint. Subsequently the 18G needle is placed centrally in the nucleus pulpous, and parallel to the endplates using posterolateral approach. Through the needle, a glass fiber is placed in the disc, enabling the application of laser energy (980 nm, 7 W, 0.6 s pulses, interval 1 second). After a total energy of 1500 J is delivered (2000 J for level L4-5), the procedure is finished, both the fiber and the needle are removed and the puncture site is covered with a sterile dressing. The patient is observed for 15 minutes before he/she can return home.
The patients were prescribed oral antibiotics for 1 day, along with bed rest for 24h. Both treatment strategies will be followed by active mobilization in the post-operative period. Early resumption of daily activities and work will be stimulated in both study groups. Monitoring of pain and disability was conducted in periods of 4 weeks, 6 weeks, 16 weeks & 24 weeks. Pain evaluation was performed using Visual Analog Scales (VAS). The measurement was assessed using a 10-point VAS with endpoint anchors of no pain (0 point) and severe pain (10 point).
Disability evaluation was performed using ODI scale. ODI is the most commonly used outcome measure for low back pain. Patient-completed questionnaire that gives a subjective percentage score of level of function (disability) in activities of daily living in those rehabilitating from low back pain. There are 10 items (pain intensity, personal care, lifting, sitting, standing, sleeping, social life, traveling, changing degree of pain). The questions are designed in a way that to realize how the back or leg pain is affecting the patient's ability to manage in everyday life [7].
At the end of week 24, patients underwent a second MRI scan to check post-PLDD change and extent of protrusion was compared with the previous one. Data analysis was performed using SPSS Version 18.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were obtained to determine the influences of each group's clinical feature to results. χ2 test, and exact fisher test were conducted to assess the overall differences between groups. Mann-Whitney and t-test was used to analyze the difference by variables between groups at each designated follow-up times. The results were considered significant at p < 0.05.
Findings: Sixty eligible participants completed the study in the course of a 6-months follow up period and were analyzed.
The mean age of all participants were 48.85 ± 14.66 (Ranging from 21 to 70) years old and male to female ratio was 2 to 1 (male: 40, female: 20). Seven patients (11.7%) reported a family history of disc herniation. The most common disc herniation level was L4-5 (53.4%) and after that L5-S1 (38.3%) and L3-4 (8.3%) respectively. Disc herniation type and location was central protrusion in 36 patients (60%) and paracentral protrusion in 24 patients (40%), (Right paracentral in 12 patients (20%) and left paracentral in 12 patients (20%). There were no statistically significant differences on the distribution in disc herniation level, type and location between two groups (p > 0.05). Patients’ demographic and clinical characteristics, sorted according to disc status, are demonstrated in Table 1.
| Variables | Patients with intact disc (N = 30 ) |
Patients with tear disc (N = 30 ) |
P-value | |
| Age (year) | 47.67 ± 13.72 | 50.03 ± 14.77 | 0.945 | |
| Gender | Male | 19 (63.3%) | 21 (70%) | 0.785 |
| Female | 11 (36.7%) | 9 (30%) | ||
| Level of protruded disc | L3-L4 | 1(3.3%) | 4 (13.3%) | 0.374 |
| L4-L5 | 17 (56.7%) | 15 (50%) | ||
| L5-S1 | 12 (40%) | 11 (36.7%) | ||
| Location of protruded disc | Central | 18 (60%) | 18 (60%) | 0.717 |
| Right paracentral | 7 (23.3%) | 5 (16.7%) | ||
| Left paracentral | 5 (16.7%) | 7 (23.3%) | ||
Table 1: Patients’ demographic and clinical characteristics.

Diagram 1: Comparison of extent of disc protrusion in two groups before procedure and at the end of follow up.
Mean extent of disc protrusion preoperatively was 5.33 ± 0.65 mm which was significantly reduced to 2.08±0.91mm at the end of follow up (p < 0.0001). Before commencing the study, mean extent of disc protrusion in patients with teared disc was 5.43 ± 0.79 mm which was reduced to 2.67 ± 0.81 mm at the end of follow up but it was not statistically significant (p = 0.24).
Mean extent of disc protrusion in patients with intact disc was 5.24 ± 0.62 mm which was reduced to 1.50 ± 0.57 mm at the end of follow up and was statistically significant (p < 0.0001).
Mean VAS was at highest level right after the procedure but was significantly reduced during the 6 months follow up period (p < 0.0001). VAS showed no statistically significant difference regarding gender, disc herniation level and location. Mean VAS in patients with teared disc was reduced at the end of follow up but it was not statistically significant (p = 0.045). Mean VAS in patients with intact disc was reduced at the end of follow up and was statistically significant (p < 0.0001).
Mean ODI was at highest level (62.25 ± 12.22) right after the procedure but was significantly reduced to 20.42 ± 10.13 during the 6 months follow up period which was statistically significant (p < 0.0001). Mean ODI in patients with either teared or intact disc was reduced at the end of follow up and was statistically significant (p < 0.0001).
Discussion
Surgery and minimally invasive techniques have been shown to improve the clinical outcomes of patients with herniated disc disease who had failed a 3-month course of adequate conservative therapy [8]. Because traditional open surgery, which has been in practice since 1934, would further weaken an already compromised posterior wall of the disc complex, such an approach may not be in the best interests of the patient with herniated disc disease [9]. Therefore, the minimally invasive therapies should be considered before resorting to traditional open surgery when patients do not respond to conservative therapies. PLDD is one of the so-called “minimally invasive” treatment methods. Minimally invasive procedures have been developed to minimize the occurrence of morbidity related to open surgery. Advantages of all minimally invasive procedures are small incision, less muscle and ligament injury, no need for general anesthesia, and short hospital stay.
It has been shown that PLDD can improve the clinical outcomes of contained lumbar disc herniation. Schenk., et al. [10] reported success rates in larger studies varying from 75% to 87%. The majority of the studies considered extrusion or sequestered disc herniation as exclusion criteria. Therefore, few studies have addressed the treatment of teared lumbar disc herniation by PLDD. Choy used PLDD to treat extruded but nonsequestered lumbar disc herniation in 2001, and achieved good pain relief in patients [6]. However PLDD seems to be more effective for patients with intact (non-teared) intervertebral protruded discs.
In the present study, mean VAS was significantly reduced from 7.38 at baseline to 2.65 at the end of 6-months follow up, which is consistent with previous studies (5, 11-14). Mean ODI score was also reduced from 62.25 at baseline to 20.42 at the end of 6-months follow up. In a study on 70 patients by McCormick., et al. a reduction of more than 30% on ODI score was noted during one-year follow up period [11].
An animal study in 2012 demonstrated that nucleoplasty has a volume-reducing effect on the lumbar nucleus pulposus in an animal model [15]. In our study, postoperative MRI scan showed a statistically significant reduction of disc volume in patients with intact discs, while this reduction was not significant in the other group statistically.
Although both VAS and ODI scores along with the extent of disc protrusion were reduced in both groups, but it seems that the presence of tearing and loss of integrity in the discs, significantly lowers the chance of response to the procedure. So far, there has been no study on the effect of disc tearing on changes in pain and disability after PLDD. This study is the first evaluation to determine the role of tearing of discs on clinical implications of PLDD. Accordingly, it is not possible to compare the results of this study with other studies.
Conclusion
PLDD showed more benefits on recovery of function and pain relief in patients with intact intervertebral herniated discs, compare to teared discs. We believe that early diagnosis and proper treatment in case of disc herniation could be a good way for providing a chance for rapid alleviation. Small sample size and the relatively short period of follow up may be addressed as limitations of this study, along with the fact that this is not a randomized clinical trial: with this publication, we demonstrated the better outcome of PLDD procedure on intact (none-teared) intervertebral herniated discs and lower rate of recovery in patients with teared discs, which confirms the necessity of treatment as soon as possible and before occurring any damage to the integrity of intervertebral discs. Also informing all patients with disintegrated herniated discs about the expected outcome is highly suggested. Yet further randomized clinical trials with larger sample size and longer periods of follow ups are recommended.
References
- Choi HS., et al. “Surgical versus Conservative Treatment for Lumbar Disc Herniation with Motor Weakness”. Journal of Korean Neurosurgical Society 54.3 (2013):183–188.
- Koes BW., et al. “Diagnosis and treatment of sciatica”. BMJ : British Medical Journal 334.7607 (2007): 1313–1317.
- Jacobs WCH., et al. “Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review”. European Spine Journal 20.4 (2011): 513–522.
- Kim SH., et al. “Clinical Outcomes of Percutaneous Plasma Disc Coagulation Therapy for Lumbar Herniated Disc Diseases”. Journal of Korean Neurosurgical Society 51.1(2012): 8–13.
- Zhao XL., et al. “Treatment of Lumbar Intervertebral Disc Herniation Using C-Arm Fluoroscopy Guided Target Percutaneous Laser Disc Decompression”. Photomedicine and Laser Surgery 30.2 (2012): 92-95.
- Choy DS. “Response of extruded intervertebral herniated discs to percutaneous laser disc decompression”. Journal of Clinical Laser Medicine & Surgery 19 (2001):15–20.
- Guillemin F., et al. “Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines”. Journal of Clinical Epidemiology 46 (1993):1417–1432.
- Dewing CB., et al. “The outcomes of lumbar microdiscectomy in a young, active population: Correlation by herniation type and level”. Spine 33.1 (2008): 33-38.
- Choy DS. “Percutaneous laser disc decompression: a 17-year experience”. Photomedicine Laser Surgery 22.5 (2004): 407-410.
- Schenk B., et al. “Percutaneous laser disk decompression: a review of the literature”. American Journal of Neuroradiology 27.1 (2006): 232–235.
- Zachary L McCormick., et al. “Percutaneous Lumbar Disc Decompression Using the Dekompressor: A Prospective Long-Term Outcome Study”. Pain Medicine 17.6 (2016): 1023–1030.
- Haufe SMW., et al. “Percutaneous laser disc decompression for thoracic disc disease: report of 10 cases”. International Journal of Medical Sciences 7.3 (2010): 155–159.
- Brouwer PA., et al. “Effectiveness of percutaneous laser disc decompression versus conventional open discectomy in the treatment of lumbar disc herniation; design of a prospective randomized controlled trial”. BMC Musculoskeletal Disorders (2009): 10-49.
- Patel VB., et al. “Interventional Therapies for Chronic Low Back Pain: A Focused Review (Efficacy and Outcomes)”. Anesthesiology and Pain Medicine 5.4(2015): e29716.
- Kasch, R., et al. “Disc Volume Reduction with Percutaneous Nucleoplasty in an Animal Model”. PLoS ONE 7.11 (2012): e50211.
Citation:
Seyed Mohammdareza Haji Seyyed Abootorabi., et al. “Effects of Percutaneous Laser Disc Decompression (PLDD) on Clinical
Outcome of Teared Vs Intact Protruded Intervertebral Discs: A Prospective Cohort Study”. Orthopaedic Surgery and Traumatology 2.1
(2018): 279-285.
Copyright: © 2018 Seyed Mohammdareza Haji Seyyed Abootorabi., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.