Dissertation
Volume 2 Issue 1 - 2018
A Population Service Evaluation of the Attention Deficit Hyperactivity Disorder Pathway of Children and Young People’s Services, Malta
1Northumberland, Tyne and Wear NHS Foundation Trust St. Nicholas Hospital Jubilee Road Gosforth Newcastle upon Tyne, NE3 3XT, UK. Mental Health Malta, Mount Carmel Hospital, Triq L-Imdina, Attard Malta ATD 9033
2Mental Health Malta, Mount Carmel Hospital, Triq L-Imdina, Attard Malta ATD 9033
3Mental Health Malta, Mount Carmel Hospital, Triq L-Imdina, Attard Malta ATD 9033
4Mental Health Malta, Mount Carmel Hospital, Triq L-Imdina, Attard Malta ATD 9033. Newcastle University, Newcastle upon Tyne, Tyne and Wear, NE1 7RU, UK
2Mental Health Malta, Mount Carmel Hospital, Triq L-Imdina, Attard Malta ATD 9033
3Mental Health Malta, Mount Carmel Hospital, Triq L-Imdina, Attard Malta ATD 9033
4Mental Health Malta, Mount Carmel Hospital, Triq L-Imdina, Attard Malta ATD 9033. Newcastle University, Newcastle upon Tyne, Tyne and Wear, NE1 7RU, UK
*Corresponding Author: Andrea Saliba, Northumberland, Tyne and Wear NHS Foundation Trust St. Nicholas Hospital Jubilee Road Gosforth Newcastle upon Tyne, NE3 3XT, UK. Mental Health Malta, Mount Carmel Hospital, Triq L-Imdina, Attard Malta ATD 9033.
Received: February 12, 2018; Published: February 18, 2018
Abstract
Background: Attention Deficit Hyperactivity Disorder (ADHD) is the commonest neurodevelopmental disorder in young people (YP) aged 5-18 years. YP with untreated ADHD are five times more likely to develop co-morbid psychiatric disorders. The aims were to carry out a population service evaluation of the assessment process and management of YP with ADHD at the Children and Young People’s Service (CYPS), Malta ages 0-16 years for 2014. Also to describe the service input, assessment and treatment of YP attending CYPS and compare to ADHD NICE guidelines 2008.
Methods: All YP diagnosed with ADHD at CYPS throughout 2014 were included. The incidence of YP with ADHD on treatment age 3-16 years in Malta was calculated. Information was collected from; i. Retrospective case file review and ii. Methylphenidate and Atomoxetine registry and compared with NICE guidelines.
Results: 136 YP were diagnosed with ADHD. The minimum 12-month incidence of ADHD on treatment (3-16 years) in Malta was 553 per 100,000. Pre-diagnosis assessments were more frequently performed by other YP services (n = 97, 71.3%, p = < 0.01). A psychiatrist or paediatrician confirmed the diagnosis in 113 (83.1%) YP. 62 (45.3%) YP were prescribed medication, 50 (36.8%) were referred for parental skills course and 55 (40.4%) for psychotherapy. The mean waiting time for the first appointment was 187.6 days (CI ± 26.9, 0-720), and 301.0 days (CI ± 34.4, 0-800) for the first specialist review.
Conclusions: The incidence for YP (3-16 years) with ADHD on treatment was lower than the US. Since most pre-diagnostic assessments were carried out by other services, this raised the question about the reliability and validity. We recommend a diagnostic multidisciplinary team meeting following the multimodal assessment to diagnose ADHD. Medication prescribing followed NICE overall however standardising non-pharmacological management is required.
Keywords: ADHD; Service development; Psychiatric practice; Community programmes; Psychopharmacology
Abbreviations: ADHD: Attention Deficit Hyperactivity Disorder; CDAU: Child Development Assessment Unit; CGAS: Children global assessment scale; CI: Confidence Interval; CYPS: Children and Young People’s Service; HoNOSCA: Health of the Nation Outcome Scale; ICD-10 – International Statistical Classification of Diseases and Related Health Problems 10th Revision; MDT: Multidisciplinary team; NICE: The National Institute for Health and Care Excellence; ODD: Oppositional defiant disorder; OT: Occupational therapist; SALT: Speech and language therapist; SPSS: Statistical Package for the Social Science; SD: Standard Deviation; YP: Young people
Background
Attention deficit hyperactivity disorder (ADHD) is amongst the most common neurobehavioral disorder to present in children and adolescents (Wilens and Spencer 97-109). ADHD is more common in boys than in girls ("Attention - Deficit/Hyperactivity Disorder."1) With a worldwide prevalence rate of 5.29% (Polanczyk ., et al.).
There is no one gene which causes ADHD, and it is believed to be due to interactions between multiple genes of small effect size (Thapar., et al. 3-16). It is understood that ADHD results from an interacting combination of genetic and environmental factors (Nigg, Nikolas, and Burt 863-873). Environmental factors such as severe neglect resulting in attachment disorders (Rutter 1-21), low birth weight, pre or post-natal insults (Johnson., et al. 453-63.e1) and nutritional deficiency were expansively shown to contribute to the development of ADHD (Freeman et al. 1954-1967).
If ADHD is under or misdiagnosed or not managed well, the prognosis for YP is poor, this means that there will be negative social, academic and vocational consequences (American Psychiatric Association). A large proportion (78%) of YP with ADHD tend to present with at least one co-morbidity, the commonest include; mood disorders (40%), substance dependence (35%), anxiety disorders (25%) (Thapar., et al. 3-16).
According to NICE guidelines 2008, a diagnosis of ADHD needs to be multimodal in approach, the requests for this are the presence of a multidisciplinary team specialised in ADHD. This involves a clinical assessment of the YP that includes behaviour and symptoms in the different domains and settings of the YP’s everyday life, a developmental and psychiatric history, observer reports and assessment of the person’s mental state. Rating scales and observations (e.g. school and/ or home visits) are valuable adjuncts but a diagnosis should not solely be based on them.
The diagnosis of ADHD is made at a MDT meeting were all the reports of the YP are brought together. This diagnosis is based on the chosen diagnostic criteria and level of function of the YP. The diagnosis is then presented together with the strengths and weaknesses of the YP together with recommendations at a feedback session, accompanied by a report to parents or carers and the YP (Kendall., et al. 751-753). Teachers may be present at feedback review if this is considered appropriate. Specific treatments have been widely researched and reviewed (Kendall., et al. 751-753).
North American guidelines suggest that both psychological and pharmacological treatment are prescribed in combination, or according to clinical judgment; were medication is used as first line treatment, with psychosocial interventions as an adjunct (American Psychiatric Association). However, NICE guidelines differ from the above, in that, the first line of treatment are psychosocial interventions (especially parent training) in all but severe cases, with medication as second line of intervention (Thapar., et al. 3-16).
The Dundee ADHD Clinical Care Pathway uses standard protocols for the assessment, titration and routine monitoring of clinical care and treatment outcomes. The pathway provides effective care in a real-world setting and has demonstrated success in the long-term management of ADHD. As with any clinical pathway, there are limitations; it is time-intensive and requires well-trained staff (Coghill and Seth 52).
According to the Tees, Esk and Wear Valleys NHS Foundation Trust pathway ("Understanding ADHD - The ADHD Pathway."1) , when the YP is referred, he or she will be assessed by a specialist team and undergo a full and comprehensive assessment of ADHD. This will include: a detailed history of presenting symptoms and co-existing conditions; a review of current medications and treatments; psychosocial, developmental, educational and mental health history; impact of symptoms on educational, psychological, social and occupational functioning; impact of symptoms on peer relationships and family life, physical/growth and developmental assessment; observation in clinic settings; YP’s view; school liaison; scoring of rating scales and developmental screening tools; assessment of the YP and family needs and history of parent/carers’ mental health. Assessment may also include: carers assessment and occupational therapy assessment (this may be included depending on needs identified by comprehensive assessment). Once this information is gathered a formulation meeting will be held with parents and all professionals involved in the YP’s assessment.
The incidence rate of YP aged 0-16 years in 2014 will be calculated. Given Malta is a small island it lands itself well for population based service evaluations and to our knowledge this is the first study of its kind to be carried out. This service evaluation looked to assess the current practice of the assessment process and management of children diagnosed with ADHD at Children and young people services (CYPS), Malta, and ages 0-16 years from January to December 2014. Furthermore the results of the assessment process will be compared to the NICE guidelines 2008 as the gold standard and other services of excellence were included such as the Dundee ADHD Clinical Care Pathway and the TEWV NHS Foundation Trust person centred pathway of care for ADHD in Children and Young People.
Methods
All patients aged 0 to16 years over a one year period referred to CYPS, from 1st January 2014 to the 31st December 2014 who were diagnosed with ADHD were included in this study. This service evaluation was carried out in two parts and permission to access case notes and national treatment registries was granted from the medical director, hospital management and the respective consultants.
Procedure
The first part of this study (Part A) aimed to calculate the incidence of YP with ADHD prescribed treatment in Malta. This was done by accessing the national register which holds the number of permits issued for treatment of ADHD in Malta in 2014. This register includes all YP aged 0 to 16 years prescribed Methylphenidate and Atomoxetine both in the public and the independent sector on the NHS formulary. The incidence was calculated using the population of YP in Malta aged 0 to 16 years from the National Statistics Office, Malta. The minimum 12 month incidence of ADHD on treatment in Malta was 553 per 100,000. The incidence was calculated from all the new permits of Methylphenidate and Atomoxetine division by the total population between 0 to 16 years.
The first part of this study (Part A) aimed to calculate the incidence of YP with ADHD prescribed treatment in Malta. This was done by accessing the national register which holds the number of permits issued for treatment of ADHD in Malta in 2014. This register includes all YP aged 0 to 16 years prescribed Methylphenidate and Atomoxetine both in the public and the independent sector on the NHS formulary. The incidence was calculated using the population of YP in Malta aged 0 to 16 years from the National Statistics Office, Malta. The minimum 12 month incidence of ADHD on treatment in Malta was 553 per 100,000. The incidence was calculated from all the new permits of Methylphenidate and Atomoxetine division by the total population between 0 to 16 years.
The second part of this study (Part B) was a retrospective case file review of all YP referred to CYPS in 2014. These were identified from a patient database and the relevant YP were included in this service evaluation. Data was collected on a password protected excel spreadsheet which was created specifically for this study so as to standardise data collection. All YP who were given a diagnosis of ADHD were selected and included in the service evaluation.
Data Collection
The demographics collected on the YP identified for this study included age, gender, locality, parental relationship status, living situation and previous involvement with YP services were collected together with the source and reason of referral. The assessment process described below will be compared to the NICE guidelines 2008 as the gold standard and other services of excellence were included the Dundee ADHD Clinical Care Pathway and the TEWV NHS Foundation Trust person centred pathway of care for ADHD in Children and Young People.
The demographics collected on the YP identified for this study included age, gender, locality, parental relationship status, living situation and previous involvement with YP services were collected together with the source and reason of referral. The assessment process described below will be compared to the NICE guidelines 2008 as the gold standard and other services of excellence were included the Dundee ADHD Clinical Care Pathway and the TEWV NHS Foundation Trust person centred pathway of care for ADHD in Children and Young People.
Quality of Assessment
The retrospective case notes review involved the quality of the assessment process that includes, assessing whether a developmental history and an in depth clinical interview focusing specifically to elicit features of ADHD were obtained from the parent or carer and the YP, and also whether a school observation was carried out. The school observation included observing the child in both a structured and non-structured environment, observing teaching strategies already in place and gathering information from the class teacher. The researchers identified whether assessments were completed by the occupational therapist (OT), speech and language therapist (SALT), psychologist and whether psychometric assessments such as the Wechsler Intelligence Scale for Children (Wechsler) or ADHD rating scales (such as the Conners’ Rating Scale (Conners) were administered.
The retrospective case notes review involved the quality of the assessment process that includes, assessing whether a developmental history and an in depth clinical interview focusing specifically to elicit features of ADHD were obtained from the parent or carer and the YP, and also whether a school observation was carried out. The school observation included observing the child in both a structured and non-structured environment, observing teaching strategies already in place and gathering information from the class teacher. The researchers identified whether assessments were completed by the occupational therapist (OT), speech and language therapist (SALT), psychologist and whether psychometric assessments such as the Wechsler Intelligence Scale for Children (Wechsler) or ADHD rating scales (such as the Conners’ Rating Scale (Conners) were administered.
Service intervention
The service evaluation also recorded the time from receiving referral to initial assessment, time from the initial assessment session to the MDT meeting, time from the case formulation to the first session with the psychiatrist or paediatrician, and the time interval from first session with the psychiatrist or paediatrician to the initiation of treatment.
The service evaluation also recorded the time from receiving referral to initial assessment, time from the initial assessment session to the MDT meeting, time from the case formulation to the first session with the psychiatrist or paediatrician, and the time interval from first session with the psychiatrist or paediatrician to the initiation of treatment.
The diagnosis of ADHD according to ICD-10 (World Health Organization), based on the multi-disciplinary feedback and taking into account all the assessments carried out, was given by a psychiatrist or paediatrician. Following diagnosis, the treatment options that were given to the YP were recorded.
Data Analysis
The data collected was analysed using SPSS. Continuous data were summarised using means, 95% confidence intervals and ranges where indicated. Nominal and ordinal data were compared with the Fisher's exact test and Pearson’s Chi Squared Test depending on the sample size.
The data collected was analysed using SPSS. Continuous data were summarised using means, 95% confidence intervals and ranges where indicated. Nominal and ordinal data were compared with the Fisher's exact test and Pearson’s Chi Squared Test depending on the sample size.
Results and Discussion
Results
317 new cases were seen at CYPS (public sector) in 2014 of which 136 YP with an average age of 7.9 years (range 3 to 15 years, SD 3.22) were diagnosed with ADHD. Demographic data is demonstrated in Table 1.
317 new cases were seen at CYPS (public sector) in 2014 of which 136 YP with an average age of 7.9 years (range 3 to 15 years, SD 3.22) were diagnosed with ADHD. Demographic data is demonstrated in Table 1.
| Demographics | Number of YP (%) | |
| Gender | Males | 95 (70%) |
| Females | 41 (30%) | |
| Location | Southern Harbour | 49 (36.3%) |
| Northern Harbour | 35 (25.7%) | |
| South Eastern | 22 (16.2%) | |
| Western | 15 (11%) | |
| Northern | 14 (10.3%) | |
| Relationship status | Married parents | 86 (63.2%) |
| Single Parents | 47 (34.6%) | |
| Accommodation | Stable home environment | 130 (95.6%) |
| Unstable environment | 6 (4.4%) | |
| Source of Referral | Referred by Paediatricians | 69 (50.7%) |
| Referred by General Practitioner | 50 (36.8%) | |
| Referred by other sources | 16 (11.8%) |
Table 1: Demographics of YP with ADHD.
27 (19.9%) YP had no previous involvement with mental health services, 97 (71.3%) were previously reviewed at the Child Development Assessment Unit (CDAU), 6 (4.4%) were seen by a psychiatrist and 5 (3.7%) by Appogg which is the social services facility on the island. The main reason for referral to CYPS were behavioural difficulties (n = 67, 49.3%), ADHD symptoms (n = 66, 48.5%) and depression (n = 3, 2.2%).
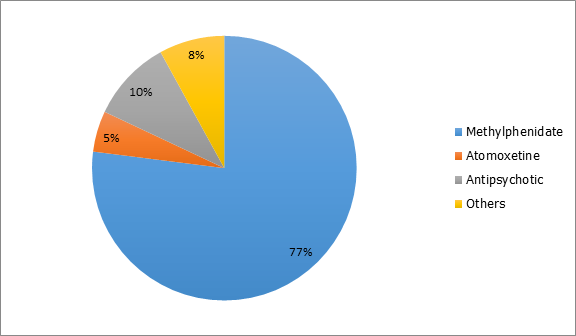
In 2014, the Malta register issued 213 Methylphenidate permits and 108 Atomoxetine permits. These included permits from both the private and public sector. The total number of new cases diagnosed with ADHD and were prescribed treatment for 2014 in Malta was 321 thus the minimum 12 month incidence of YP (age 3-16 years) with ADHD on treatment in Malta was 553 per 100,000 (0.55%) in 2014.
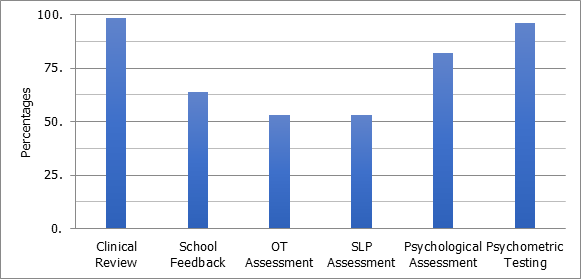
A psychosocial assessment and developmental history was obtained in 134 (98.5%) of patients who attended the public sector, however no (0%), specific ADHD neurodevelopmental assessments were recorded. At the intake MDT meeting, it was reported that 131 (96.3%) of YP had psychometric testing carried out and 87 (64.0%) of the YP had received feedback from their school. Psychometric testing by CYPS was carried out more frequently in those not previously assessed at CDAU (p = 0.02).
Of the YP diagnosed with ADHD, 72 (52.9%) received OT assessments, 72 (52.9%) SALT assessments and 111 (82.2%) received psychological assessments. Psychological, OT, SALT, school feedback assessments were more frequently carried out in YP previously attending CDAU rather than those assessed by CYPS only (n = 97, 71.3%, p = < 0.01).
Following the intake MDT, 113 (83.1%) YP were assessed by a specialist psychiatrist or paediatrician of whom received a diagnosis of ADHD based on NICE guidelines 2008: clinical and psychosocial assessment, full developmental and psychiatric history and observer reports and assessment. The rest (n = 23, 16.9%) were given a diagnosis by a non-ADHD specialist, these were psychiatric trainees.
After receiving a diagnosis of ADHD, 55 (40.4%) were referred for psychological therapy, the modality of therapy was not specified. 50 (36.8%) were referred to a parental skills course offered by another service (the type of parental skills was not specified), 7 (5.2%) referred for OT and the school was involved in 13 (9.6%) of YP.
At intake 38 (27.9%) YP were already prescribed psychiatric treatment. This number increased to 62 (45.6%) following assessment, these medications included methylphenidate (n = 48, 35.3%), an antipsychotic (n = 6, 4.4%), atomoxetine (n = 3, 2.2%), others medications included e.g. tricyclic antidepressants (n = 5, 3.7%). Of those YP prescribed treatment a physical examination was carried out in; blood pressure and pulse in 24 (32.9%) YP, 59 (80.8%) and 58 (79.5%) had their weight and height monitored respectively. 49 (67.1%) had an ECG taken although this was done regardless whether the patient had a personal or family history of heart disease. 30 (22%) YP were found to have a co-morbid psychiatric disorder; 8.8% oppositional defiant disorder (ODD), 4.4% anxiety, 3.7% conduct disorder, 2.9% autism spectrum disorder, 1.5% depression and 0.7% obsessive compulsive disorder.
Service Input
The mean waiting time from referral to initial assessment was 187.6 days (95% confidence interval [CI] ± 26.9, range 0-720). To account for the long waiting time, a nurse based triage system is in place, urgent cases are offered an initial assessment within a week. The average waiting time from initial assessment to the initial MDT meeting was 15.1 days (95% confidence interval [CI] ± 6.3, range 0-280). Patients waited an average of 105 days (95% confidence interval [CI] ± 15.9, range 0-483) from the MDT to the first session with the psychiatrist and 301.0 days (CI ±34.4, range 0-800) from referral to first specialist review. The mean time interval from first session with the specialist to initiation of medication was 60.5 days (95% confidence interval [CI] ± 24.0, range 0-406).
The mean waiting time from referral to initial assessment was 187.6 days (95% confidence interval [CI] ± 26.9, range 0-720). To account for the long waiting time, a nurse based triage system is in place, urgent cases are offered an initial assessment within a week. The average waiting time from initial assessment to the initial MDT meeting was 15.1 days (95% confidence interval [CI] ± 6.3, range 0-280). Patients waited an average of 105 days (95% confidence interval [CI] ± 15.9, range 0-483) from the MDT to the first session with the psychiatrist and 301.0 days (CI ±34.4, range 0-800) from referral to first specialist review. The mean time interval from first session with the specialist to initiation of medication was 60.5 days (95% confidence interval [CI] ± 24.0, range 0-406).
Discussion
This was the first service evaluation carried out to date of the Maltese population attending CYPS. From the findings reported the incidence for YP aged 3-16 years diagnosed with ADHD and receiving medication in Malta (0.55%) was lower than the US, which had an incidence of 4.2-14.8% in 2011 for ages 4-17 years (Centers for Disease Control and Prevention (CDC 842). On the one hand, this could be that Malta is under diagnosing and under treating ADHD, this could possibly be the result of less awareness and more stigma (Camilleri and Makhoul). On the other hand, this may be a result of issues to do with diagnostic criteria used (ICD-10 and DSM-IV) and the quality of the methodology of epidemiological studies carried out (Polanczyk., et al.).
It was noticed that most psychometric assessments were carried out by other services outside of CYPS. The authors raised the question about the reliability and validity of the pre-diagnostic assessments. From the results, the CDAU carried out multidisciplinary assessments then referred the YP to CYPS for further assessments and treatment. This duplication of work can result in delays in accessing treatment and prolonging the YP and care givers anxiety. Gerralda., et al. 2016 (Garralda and Slaveska‐Hollis 96-101) recommends joint child and adolescent paediatric and mental health services to reduce the duplication of the assessment process and the need to depend on outsourcing assessments from other services.
A multimodal assessment with a neurodevelopmental history and school observation (following a standardised proforma), as indicated by NICE 2008, followed by a MDT meeting to discuss the diagnosis and management as recommended by the TEWV person centred pathway of care for ADHD were not carried out at CYPS. An ad hoc assessment by the specialist and the developmental history taken by the mental health worker were carried out. The authors recommend setting up a standardised pathway of assessment and intervention that includes a multimodal assessment, diagnosis and management.
No documentation for categorization of level of severity into mild, moderate or severe ADHD as recommended by NICE was carried out in order to decide on the treatment pathway indicated. This may be due to time constraints experienced by psychiatrists and paediatricians in view of a low patient to staff ratio and the lack of a standardized treatment pathway requesting categorisation. Stratifying patients into the degree of severity would allow more efficient use of resources and ensure that the service provides an individual tailored care plan for the YP following NICE. The type of medication prescribed followed NICE in most cases, although a higher than expected use of antipsychotic treatment was noted, this is possibly used to control symptoms of co-morbid conduct disorder, patients being misdiagnosed and treatment options not being influenced by recommended guidelines.
Standardising non-pharmacological management is required by documenting the type of psychological intervention, waiting times to start therapy and the number of sessions provided (Kendall., et al. 751-753). Since the type of psychological intervention offered by CYPS was not documented, this could not be compared to the recommendations made by NICE, which are CBT and/or social skills training. The authors recommend having in house parent training and education programmes which are evidence based (Sonuga-Barke., et al. 275-289), as at the time of service evaluation these were being outsourced from other services. Multiple random control trials have shown that The Incredible Years Parent, Teacher, and Child Training Programs is effective in encouraging positive parental skills, building the child’s social, emotional, and self-regulation competence and decreasing behavioural difficulties (Webster-Stratton ).
CYPS waiting times did not follow guidelines, according to the LDP Standards target in NHS Scotland, a child should not wait for more than 18 weeks (Hookway and Lead) from referral to treatment in CAMHS.
Conclusions
The authors recommend that a follow up service evaluation is carried out after the introduction of: a multimodal method of assessment and diagnosis, parental skills groups at CYPS, methylphenidate XL preparation available on the NHS formulary and documentation of psychological modality and degree of ADHD severity. We suggest the use of objective assessment scales such as the Connors or Swanson, Nolan andPelham questionnaire and outcome measures such as the children global assessment scale (CGAS) (Shaffer., et al. 1228-1231), Health of the Nation Outcome Scale (Gowers., et al. 413-416) and side effect profile template to assess the response to treatment and side effect monitoring (McDonagh., et al.). The latter is important to monitor progress and be alerted to side effects to improve outcomes and treatment compliance. In order to provide holistic care and develop a patient centred service, we suggest carrying out service user satisfaction questionnaire and implementing changes according to the outcomes results.
A move from having a number of different YP services working individually to one larger streamlined service with professionals working in collaboration together may be the next step to develop evidence based and standardised service. This would help to reduce waiting times from referral to treatment to less than 18 weeks with the aim to improve the standard of assessment and management of ADHD by CYPS.
Conflicts of interest
The authors have declared that they have no competing or potential conflicts of interest.
The authors have declared that they have no competing or potential conflicts of interest.
References
- American Psychiatric Association. “American Psychiatric Association Practice Guidelines for the Treatment of Psychiatric Disorders: Compendium 2006”. American Psychiatric Pub, (2006).
- Camilleri., et al. "ADHD: From Childhood into Adulthood”. Malta Medical Journal 25.1(2013).
- Centers for Disease Control and Prevention (CDC). "Mental Health in the United States. Prevalence of Diagnosis and Medication Treatment for Attention-Deficit/Hyperactivity Disorder--United States, 2003”. MMWR Morbidity and mortality weekly report 54.34 (2005): 842-847.
- Coghill David and Sarah Seth. "Effective Management of Attention-Deficit/Hyperactivity Disorder (ADHD) through Structured Re-Assessment: The Dundee ADHD Clinical Care Pathway”. Child and adolescent psychiatry and mental health 9.1 (2015): 52.
- Conners C Keith. Conners' Rating Scales Revised. Multi-Health Systems, Incorporated, (2001).
- Freeman Marlene P., et al. "Omega-3 Fatty Acids: Evidence Basis for Treatment and Future Research in Psychiatry”. Journal of Clinical psychiatry 67.12 (2006): 1954-1967.
- Garralda M Elena and Karmen Slaveska‐Hollis. "What is Special about a Paediatric Liaison Child and Adolescent Mental Health Service?" Child and Adolescent Mental Health 21.2 (2016): 96-101.
- Gowers Simon G., et al. "Brief Scale for Measuring the Outcomes of Emotional and Behavioural Disorders in Children: Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA)”. The British Journal of Psychiatry 174.5 (1999): 413-416.
- Hookway Gavin,and Senior Quality Improvement Lead. "Highland Nhs Board”. Print.
- Johnson S., et al. "Psychiatric Disorders in Extremely Preterm Children: Longitudinal Finding at Age 11 Years in the EPICure Study”. Journal of the American Academy of Child and Adolescent Psychiatry 49.5 (2010): 453-463.
- Kendall Tim., et al. "Guidelines: Diagnosis and Management of Attention-Deficit/Hyperactivity Disorder in Children, Young People, and Adults: Summary of NICE Guidance”. BMJ: British Medical Journal 337 (2008): 751-753.
- McDonagh, M. S., et al. (2011) Print.
- Nigg J., et al. "Measured Gene-by-Environment Interaction in Relation to Attention-Deficit/Hyperactivity Disorder." Journal of the American Academy of Child and Adolescent Psychiatry 49.9 (2010): 863-873.
- Polanczyk Guilherme., et al. "The Worldwide Prevalence of ADHD: A Systematic Review and Metaregression Analysis”. American journal of psychiatry 164.6 (2007): 942-948.
- Rutter Michael. "Nature, Nurture, and Development: From Evangelism through Science toward Policy and Practice”. Child development 73.1 (2002): 1-21.
- Shaffer David., et al. "A Children's Global Assessment Scale (CGAS)”. Archives of General Psychiatry 40.11 (1983): 1228-1231.
- Sonuga-Barke Edmund JS., et al. "Nonpharmacological Interventions for ADHD: Systematic Review and Meta-Analyses of Randomized Controlled Trials of Dietary and Psychological Treatments”. American Journal of Psychiatry 170.3 (2013): 275-289.
- Thapar Anita., et al. "Practitioner Review: What have we Learnt about the Causes of ADHD?" Journal of Child Psychology and Psychiatry 54.1 (2013): 3-16.
- Webster-Stratton Carolyn. "Quality Training, Supervision, Ongoing Monitoring, and Agency Support: Key Ingredients to Implementing the Incredible Years Programs with Fidelity." Washington: University of Washington (2004).
- Wechsler David. Wechsler Intelligence Scale for Children-WISC-IV. Psychological Corporation (2003).
- Wilens Timothy E and Thomas J Spencer. "Understanding Attention-Deficit/Hyperactivity Disorder from Childhood to Adulthood." Postgraduate medicine 122.5 (2010): 97-109.
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research. 2 Vol. World Health Organization, (1993).
Citation:
Andrea Saliba., et al. “A Population Service Evaluation of the Attention Deficit Hyperactivity Disorder Pathway of Children and
Young People’s Services, Malta”. Chronicles of Pharmaceutical Science 2.1 (2018): 453-461.
Copyright: © 2018 Andrea Saliba., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.