Research Article
Volume 2 Issue 1 - 2018
Spontaneous Breathing Trial across Intensive Care Units: Delivers Safer Care and Reduces Practice Variation among Intensivists
University of Miami Miller School of Medicine USA
*Corresponding Author: Tanira Ferreira MD, University of Miami Miller School of Medicine USA.
Received: July 10, 2018; Published: July 17, 2018
Abstract
Prolonged endotracheal intubation and premature weaning can lead to complications and increased morbidity and mortality in intensive care unit (ICU) patients. The approach to discontinuing mechanical ventilation varies among practitioners. The purpose of this study was to decrease variation and standardize care by implementing a respiratory therapist and nurse driven evidence-based spontaneous breathing trial (SBT) protocol to identify patients ready for extubation. Variables collected included number of SBTs performed, failure rate of SBTs, rates of extubation and reintubation, ICU length of stay (ICU LOS), mortality and ventilator acquired pneumonias (VAP). Results from year 1 versus year 3 demonstrated a trend towards decreased ventilator days (3031 vs 2784), decreased reintubations (5% vs 2%), and increased number of successful SBTs (52% vs 58%) and extubations (48% vs 76%). ICU LOS, mortality, and VAP was similar. This protocol can be safely implemented, promotes collaboration among ICU members, and eliminates variation in weaning and extubation practices.
Introduction
The complications associated with mechanical ventilation, especially when used for prolonged time, are well established. These complications are associated with worsening morbidity and mortality [1,2]. Therefore, it becomes paramount to minimize the amount of time patients are subjected to invasive positive pressure ventilation and to liberate them from mechanical ventilation as soon as their condition allows.
There has been great debate as to which weaning method is the most effective one. Studies designed in long-term care facilities with patients requiring prolonged ventilation have failed to consistently show a method that seems to be more effective [3-6]. However, it appears that the institution of a well-defined protocol, independent of the weaning mode utilized, leads to improved outcomes when compared to the lack of a standardized protocol [7-11].
In intensive care units (ICUs) where patients are acutely ill and often require short-term mechanical ventilation, it becomes of extreme importance to promptly identify those that could potentially be liberated from the ventilator. By decreasing time spent on invasive positive pressure ventilation, the associated risks also decrease, thereby decreasing its associated morbidity and mortality and hospitalization costs.
The health care system has changed over the past few decades in such a way that there is increased emphasis on a multidisciplinary approach across healthcare. This may be highlighted when it comes to critically ill patients requiring mechanical ventilation. The role of nursing staff and respiratory therapists is crucial in identifying patients who qualify for spontaneous breathing trials. The implementation of a standardized protocol designed to identify such patients and to alert physicians when patients meet the predefined criteria has been shown to improve outcomes [8-11].
We recognized at our facility that there was a significant variation in practice patterns among intensities when it came to the approach of liberating patients from mechanical ventilation. In order to address this, we designed a respiratory therapist and nurse driven protocol that aimed to identify the ICU patients that were potentially ready for extubation. Our objectives were to implement a systematic approach to spontaneous breathing trials and liberation from the ventilator, to minimize human error and physician bias and to integrate best-evidence rules across all intensive care units in the hospital.
Methods
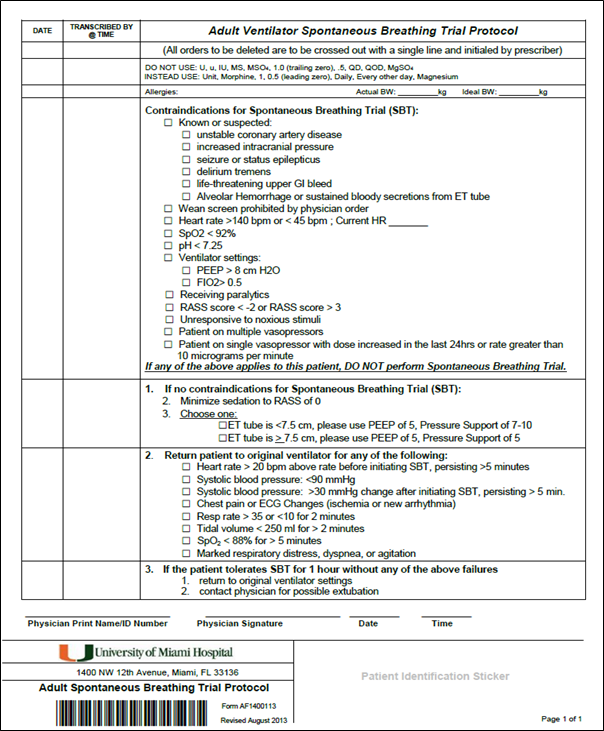
This quality improvement project was conducted in a university-owned, multi-specialty, acute care hospital during the fiscal years of 2014-2016. The hospital has 450 beds, with 52 intensive care unit beds. Our weaning protocol was created based on published protocols and current literature [8-11] (see Figure 1). Patients within the medical, surgical, cardiac and neurosurgical ICUs requiring mechanical ventilation for greater than 24 hours were included. Patients with respiratory failure on the ventilator for more than 7 days, tracheostomy, or do not resuscitate/do not intubate orders were excluded.
Starting in the year 2014, the protocol was placed in the chart of patients on the day of intubation. Prior to the protocol start date, we dedicated three months to training and educating of respiratory therapists, nursing staff and physicians on the protocol triggers and process. Once the protocol was in place, its use was reinforced during multidisciplinary rounds on a daily basis. At the end of night shift, respiratory therapy and nursing staff evaluated each patient to determine eligibility for inclusion in the protocol.
The protocol was derived from existing data [12-15]. Patients were assessed for contraindications for spontaneous breathing trial (SBT) such as known or suspected unstable coronary artery disease, increased intracranial pressure, seizure or status epilepticus, among others (view table 1).
| Contraindications for Spontaneous Breathing Trials |
| 1. Known or suspected unstable coronary artery disease |
| 2. Increased intracranial pressure |
| 3. Seizure or status epilepticus |
| 4. Delirium tremens |
| 5. Life-threatening upper gastro-intestinal bleed |
| 6. Alveolar hemorrhage or sustained bloody secretions from endotracheal tube |
| 7. Screening prohibited by physician order |
| 8. Heart rate greater than 140 beats per minute or less than 45 beats per minute |
| 9. Oxygen saturation (SpO2) less than 92% |
| 10. pH less than 7.25 |
| 11. Ventilator settings that include PEEP greater than 8 or FiO2 greater than 50% |
| 12. Current use of neuromuscular blockers |
| 13. Richmond Agitation-Sedation Scale (RASS) less than negative 2 or greater than 3 |
| 14. Unresponsiveness to noxious stimuli |
| 15. Use of multiple vasopressors |
| 16. Use of single vasopressor with dose increase in the last 24 hours |
Table 1: Contraindications for Spontaneous Breathing Trials.
If no contra-indications were found, sedation was minimized to achieve a Richmond Agitation and Sedation Scale of 0. Patients then underwent SBT prior to morning physician rounds, with use of pressure support and positive end expiratory pressure (PEEP) based on endotracheal tube size.
Patients were returned to original ventilator settings if one of the following occurred: heart rate increased by 20 beats per minute above initial rate for more than 5 minutes; systolic blood pressure (SBP) less than 90 mmHg or an increase in SBP of more than 30 mmHg above baseline for more than 5 minutes; chest pain or electrocardiogram changes indicating new arrhythmia or ischemic changes; respiratory rate less than 35 or greater than 10 for greater than 2 minutes; SpO2 < 88% for more than 5 minutes; marked respiratory distress, dyspnea or agitation.
If patients tolerated the SBT for at least one hour, the ICU physician of record was notified and decided if the patient should be extubated.
Data collection
For all patients included in the project, data from protocol and medical records was collected daily and analyzed based on calendar year. Data from medical, surgical, cardiac and neurosurgical intensive care units was obtained and grouped together.
For all patients included in the project, data from protocol and medical records was collected daily and analyzed based on calendar year. Data from medical, surgical, cardiac and neurosurgical intensive care units was obtained and grouped together.
The information collected included number of ventilator-days, number of spontaneous breathing trials performed, success rate of SBTs, failure rate of SBTs, rate of extubation, and rate of re-intubation.
In addition, the ICU length of stay (LOS), ICU mortality, and number of ventilator acquired pneumonias (VAP) were analyzed based on calendar year through hospital administrative records.
Overall patient acuity was measured by the case mix index (CMI). CMI was originally designed to measure the relative cost or resources needed to treat a certain patient population and to calculate hospital payments [16]. However, it has also been used as a marker of disease severity, particularly since 2007 with the introduction of the Medicare Severity Diagnosis Related Groups (MS-DRG) to capture disease severity more accurately by the Centers for Medicare and Medicaid Services (CMS).
Results
The CMI for patients in the ICU was 3.00 in 2014, 3.04 in 2015 and 3.03 in 2016. The ICU LOS was 3.6 days in 2014, 3.8 in 2015 and 4.1 days in 2016. The ICU mortality for all patients was 8.2% in 2014, 8.3% in 2015 and 8.9% in 2016. The ICU mortality for patients that required mechanical ventilation was 20.6% in 2014, 20.7% in 2015 and 20.2% in 2016. The VAP rate in 2014 was 0.26 per 1,000 ventilator days, 0.37 in 2015 and 0.40 in 2016. (View table 2).
| CMI, ICU LOS and mortality, Ventilator mortality, VAP rate per year | |||
| 2014 | 2015 | 2016 | |
| CMI | 3.00 | 3.04 | 3.03 |
| ICU LOS | 3.6 | 3.8 | 4.1 |
| ICU Mortality | 8.2% | 8.3% | 8.9% |
| Mechanical Ventilation Mortality | 20.6% | 20.7% | 20.2% |
| VAP (per 1,000 ventilator days) | 0.26 | 0.37 | 0.4 |
Table 2: CMI: Case Mixed Index; ICU LOS: Intensive Care Unit length of stay;
VAP: ventilator acquired pneumonia.
VAP: ventilator acquired pneumonia.
In the first year the protocol was implemented, 2014, there were a total of 3031 ventilator days. During that year, 1086 SBTs were performed (36%). Of those SBTs performed, 564 met criteria for success. Of the patients that passed the SBT, 270 were extubated (48%). The remaining patients were not extubated due to physician order. The reintubation rate was 5% (14 patients out of 270) (table 3).
| Ventilator days, number of SBTs, successful SBTs, extubations and reintubations per year | |||
| 2014 | 2015 | 2016 | |
| Ventilator-days | 3031 | 2953 | 2784 |
| Number of SBTs | 1086 (36%) | 1399 (47%) | 1149 (41%) |
| Successful SBTs | 564 (52%) | 748 (53%) | 666 (58%) |
| Extubations | 270 (48%) | 237 (32%) | 509 (76%) |
| Reintubations | 14 (5%) | 20 (8%) | 9 (2%) |
Table 3: (SBT) spontaneous breathing trial.
In 2015, the percentage of SBTs performed increased to 47% (1399 cases out of 2953). A similar amount of patients passed the SBT (748 out of 1399, or 53%). However, only 32% of those patients who passed the SBT were extubated (32%). The reintubation rate remained low at 8% (20 cases out of 237) (table 3).
In 2016, we observed a SBT rate of 41% (1149 out of 2784). 58% of patients passed the SBT (666 cases out of a total of 1149). We observed an increase in the extubation rate for the final year of data collection, and of 666 patients that passed the SBT, 509 were extubated (76%). The reintubation rate was the lowest for the three years at only 2% (9 cases out of 509) (table 3).
Discussion
Prompt identification of critically ill patients who have recovered from respiratory failure and are ready to be liberated from mechanical ventilation is paramount. Our study demonstrates that a protocol approach compares favorably when benchmarking against extubation and reintubation rates in similar patients and units.
The study was not designed to measure weaning duration in hours, total duration of individual patients on the ventilator, ICU LOS, ventilated patients mortality or VAP reduction, but rather to reduce unnecessary variation in mechanical ventilation and extubation practices within sub-specialized ICUs. Moreover, the authors believe such practice allows a better focus in identifying and treating high-risk patients.
There was likely reduced initial adherence to the protocol, and we believe that adherence increased as intensivists, respiratory therapists and nursing staff became more familiar and comfortable with the protocol. In addition, our patient population was different across the sub specialized ICUs, which contributed to the variability in outcomes.
Prolonged mechanical ventilation leads to increased associated complications including VAPs. Therefore the rapid identification of those patients who are ready to be liberated from the ventilator becomes of vital importance. Our study demonstrated a trend towards a reduction in total ventilator days, and a higher extubation rate with lower reintubation rate particularly in year 2016. This is likely explained by an increased adherence to the protocol.
We did not observe reduction in ICU LOS, mechanical ventilation mortality and VAP. However, the study was not prospectively designed to collect this information.
Previous studies that compared a standardized protocol against usual care (no protocol) have shown that the benefits above can be achieved with no harm to the patients [8-17]. In our study, we noted a trend towards improved ability to recognize patients who were ready to undergo spontaneous breathing trials and be extubated, as noted in the final year of analyzed data. Due to positive results and no side effects observed, the spontaneous breathing trial protocol was incorporated readily into our hospital staff’s routine and is now part of the usual care.
This initiative promotes an interdisciplinary collaboration in which respiratory therapists and nurses are actively involved in the ventilator liberation process and are key members in the success of this strategy. The daily commitment of time from the physicians in the implementation of the protocol was minimal, and the daily screening tests and trials required only a few additional minutes per patient per day.
Other centers [8-17] have experienced similar success. Both community and university based hospitals across the country can benefit from similar strategies. The authors also recognize extubation is not the end point and additional therapies for a successful hospitalization with improved patient outcomes are needed.
This study had several limitations. We do not have sufficient data to compare the rate of spontaneous breathing trials and extubations for the ICUs before the protocol was implemented. Data collection does not allow us to separate patients from the different intensive care units, therefore our results cannot be individualized to specialty specific units.
Adherence to the protocol increased with time, and we are not able to control our results to different periods of time and protocol adherence.
Our study saw a re-intubation rate that is lower than what most literature shows [4-20]. The median rate of re-intubation observed in interventional and observational studies is 14%. For the last year of analyzed data, our rate of failed extubation was 2%. This low rate potentially suggests that intensivists in our hospital are conservative when it comes to extubating patients.
Additional reasons for not extubating patients who passed the SBT included the amount of secretions, altered mental status, weak cough, among others, and physician direct order. There was a significant variability in management of patients in the different units given that we have different intensivists, with different backgrounds and training. The implementation of this standardized protocol reduced this variability and physician bias and instilled evidence-based practice into our critical care units.
Conclusions
A respiratory therapist and nursing driven spontaneous breathing trial protocol can be successfully and safely implemented accross different subspecialized intensive care units becoming part of usual care. Our protocol promotes collaboration among ICU team members and eliminates unnecessary variation in weaning and extubation practices.
We observed an increase in extubation and reduction in reintubation rate with implementation of a spontaneous breathing trial protocol, however that does not necessarily translate into improved patient outcomes. Further studies are necessary to determine whether such protocols also reduce ICU and hospital mortality and duration of mechanical ventilation.
Declaration of Conflicting Interests
The Authors declares that there is no conflict of interest.
The Authors declares that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Chatila., et al. "Complications of long-term mechanical ventilation". Respiratory Care Clinics of North America 8.4 (2002): 631-647.
- Klompas M. "Complications of mechanical ventilation-the CDC's new surveillance paradigm". The New England Journal of Medicine 368.16 (2013): 1472-1475.
- Brochard L., et al. "Comparison of three methods of gradual withdrawal from ventilatory support during weaning from mechanical ventilation". American Journal of Respiratory and Critical Care Medicine 150.4 (1994): 896-903.
- Esteban A., et al. "A comparison of four methods of weaning patients from mechanical ventilation Spanish Lung Failure Collaborative Group". The New England Journal of Medicine 332.6 (1995): 345-350.
- Vitacca M., et al. "Comparison of two methods for weaning patients with chronic obstructive pulmonary disease requiring mechanical ventilation for more than 15 days". American Journal of Respiratory and Critical Care Medicine 164.2 (2001): 225-230.
- Jubran A.,et al. "Effect of pressure support vs unassisted breathing through a tracheostomy collar on weaning duration in patients requiring prolonged mechanical ventilation: a randomized trial". Journal of the American Medical Association 309.7 (2013): 671-677.
- Kollef MH.,et al. "A randomized, controlled trial of protocol-directed versus physician-directed weaning from mechanical ventilation". Critical Care Medicine 25.4 (1997): 567-574.
- Marelich GP., et al."Protocol weaning of mechanical ventilation in medical and surgical patients by respiratory care practitioners and nurses: effect on weaning time and incidence of ventilator-associated pneumonia". Chest 118.2 (2000): 459-67.
- Krishnan JA., et al. "A prospective, controlled trial of a protocol-based strategy to discontinue mechanical ventilation". American Journal of Respiratory and Critical Care Medicine169.6 (2004): 673-678.
- Roh JH., et al. "A weaning protocol administered by critical care nurses for the weaning of patients from mechanical ventilation".Journal of Critical Care 27.6 (2012): 549-555.
- Danckers M., et al."Nurse-driven, protocol-directed weaning from mechanical ventilation improves clinical outcomes and is well accepted by intensive care unit physicians". Journal of Critical Care 28.4 (2013): 433-341.
- Krieger BP., et al. "Evaluation of conventional criteria for predicting successful weaning from mechanical ventilatory support in elderly patients". Journal of Critical Care 17.9 (1989): 858-861.
- Ely EW., et al. "The prognostic significance of passing a daily screen of weaning parameters". Intensive Care Medicine 25.6 (1999): 581-587.
- MacIntyre NR., et al. "Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine". Chest 120.6 (2001): 375-395.
- Girard TD., et al. "Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): a randomised controlled trial". Lancet 371.9607(2008): 126-314.
- Mendez CM., et al."Impact of hospital variables on case mix index as a marker of disease severity". Popul Health Management17.1(2014): 28-34.
- Blackwood B., et al."Protocolized versus non-protocolized weaning for reducing the duration of mechanical ventilation in critically ill adult patients". Cochrane Database System Revision11 (2014): CD006904.
- Tobin MJ., et al."The pattern of breathing during successful and unsuccessful trials of weaning from mechanical ventilation". The American Review of Respiratory Disease Returns 134.6 (1986): 1111-1118.
- Bien MY., et al. "Comparisons of predictive performance of breathing pattern variability measured during T-piece, automatic tube compensation, and pressure support ventilation for weaning intensive care unit patients from mechanical ventilation". Journal of Critical Care 39.10 (2011): 2253-2262.
- Thille AW., et al. "Outcomes of extubation failure in medical intensive care unit patients". Journal of Critical Care 39.12 (2011): 2612-2618.
Citation:
Tanira Ferreira., et al. “Spontaneous Breathing Trial across Intensive Care Units: Delivers Safer Care and Reduces Practice
Variation among Intensivists”. Pulmonary Research and Respiratory Care 2.1 (2018): 134-141.
Copyright: © 2018 Tanira Ferreira., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
















 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.