Research Article
Volume 7 Issue 1 - 2022
Alzheimer's Disease: A Path To a Cure
Professor, International Institute of Medicine & Science, California, U.S.A.
*Corresponding Author: Dr. Alain L. Fymat, Professor, International Institute of Medicine & Science, California, U.S.A.
Abstract
Abstract: In earlier publications, I posited that Alzheimer's disease is but a runaway autoimmune disease as we age and that the compromised integrity of the blood-brain barrier is not a component of the etiology of the disease. Any effective treatment for Alzheimer's (and other neurodegenerative diseases/disorders) should involve the rebalancing of the antagonistic hyper-excited synaptoblastic (synapse-building) pressures and the depressing synaptoclastic (synapse-dismantling) pressures by regulating the brain's immune system (a conflict resolution issue). The brain's immune system is an ally, not an enemy, in the battle against Alzheimer's disease. Likewise, the peripheral (or body's) immune system plays a larger role in the disease than previously thought. The amyloid-beta plaques are not the root cause of the disease (only one of its symptoms) and their clearing does not treat (or contribute to treat) the disease but may, in certain cases, even worsen it. Further, Alzheimer's is not an inflammatory disease and indeed Alzheimer's drugs that target inflammation in the brain have failed to show any benefit. Still further, the microglia seem to protect the brain by “corralling” the amyloid plaques, thus actually acting as a physical barrier that slows the expansion of plaques and blocks the ability of free-floating amyloid-beta proteins to bind to the plaques and cause toxicity. Improving the microglia's shielding function, it is possible to reduce toxicity to neurons. Because of its side effects and possible generation of other autoimmune diseases, therapeutic vaccination could only be employed under certain conditions (limiting its stimulation of the immune system, foregoing its adjuvant components). Stem cell therapy could also be considered provided any preliminary radiation treatment (if needed, such as to kill previous cancerous cells) and employing autologous stem cells (to avoid targeting the indigenous stem cells by considering them as foreign bodies). Being a complex disease, some or all of the above therapies might conceivably be needed to eradicate the disease.
Keywords: Alzheimer's disease; Amyloid plaques; Autoimmune diseases; Autologous stem cells; Brain immune system; Brain protective barriers; Inflammation; Neurodegenerative diseases; Peripheral immune system; Therapeutic vaccination
Abbreviations: Aβ: Amyloid-beta (a protein); AD: Alzheimer's Disease; ALS: Amyotrophic Lateral Sclerosis; APP: Amyloid Precursor Protein; BBB: Blood-Brain Barrier; BCSFB: Blood-CerebroSpinal Fluid Barrier; BPB: Brain Protective Barriers; CAR: Chimeric Antigen Receptor; CNS: Central Nervous System; CTLA: Cytotoxic T-Lymphocyte Antigen; DESS: Diet, Exercise, Stress, Sleep; EOFD; Early Onset Familial Disease; Ig: Immunoglobulin; LOD: Late-Onset Disease; MHC: Major Histocompatibility Complex; MS: Multiple Sclerosis; NDD: NeuroDegenerative Disorder/Disease; NFT: NeuroFibrillary Tangles; NP: NanoParticle; NT: NanoTechology; PD: Programmed Death; PD: Parkinson's Disease; PSC: Pluripotent Stem Cell; RBB: Retinal-Brain Barrier; SC: Stem Cell; SD: Sporadic Disease.
Background and Introduction
Over the past few decades, Alzheimer's disease (AD), once considered a rare disorder, has emerged from obscurity to become a major public health problem. Based on a lack of treatment, it has generally been considered as an irreversible, progressive brain disease that slowly destroys memory and thinking skills, eventually even the ability to carry out the simplest tasks. It is a chronic neurodegenerative disorder (NDD) of poorly (or not) understood cause(s). Based on identified risk factors, several theories (hypotheses) have been propounded for its cause(s). The hypotheses can be classified as: cholinergic, amyloid-beta (Aβ) protein, tau protein, viral or fungal infection, neurovascular, neuroinflammation, neurodevelopmental, cardiovascular, gum disease infection, dysfunction of oligodendrocytes, etc. Other hypotheses are related to lifestyle, diet, and the environment. (For a run down of these hypotheses, see Chapter 6 of Fymat, 2019h). Such a wide array of hypotheses is by itself indicative of our lack of true understanding and knowledge of the disease notwithstanding the fact that the disease has been identified since 1901, has been the subject of a considerable number of publications dealing with it (in excess of 50,000 articles according to some authors), hundreds of failed clinical trials, and billions of dollars spent worldwide. In the absence of medical breakthroughs, 152 million people are predicted to develop the illness by 2050, with a worldwide cost projected to reach $2 trillion by 2030!
Notwithstanding claims by some research clinicians, there are currently no known and accepted treatments if only to stop or reverse the progression of the disease. Some of these alleged treatments, including the advocated program DESS (Diet, Exercise, Stress, Sleep), and variations on this theme, are palliative in nature, temporarily improving symptoms,... while the disease progresses unabated. One must keep in mind that these programs address risks, but risk is not causation and risk management is not treatment, … only palliation!
Lacking advances in curative treatment, research has therefore been refocused on diagnosing the condition before symptoms begin. Thus, a number of biochemical tests have been developed to attempt earlier detection. Such tests include the analysis of the cerebrospinal fluid for Aβ or tau proteins and preventive vaccination. Neuroprotective agents (such as Al-108, PBT2, and TNFα receptor-blocking fusion protein etarnacept) have also been mentioned.
Further, among the more than 400 pharmaceutical treatments having been investigated or are in advanced clinical trials, putative pharmaceutical therapies attempt to treat the underlying disease pathology by reducing the levels of Aβ in the plaques (for example, by Apomorphine, vaccination). Such treatments also include inhibiting tau-aggregation in the neurofibrillary tangles (NFT), e.g., with Methylthionium chloride and Dimebon. However helpful, such treatments are likewise not curative. Now, … what is going on?
Have We Got The Cause of Ad All Wrong?
As known, in 1901, Dr. Alois Alzheimer first described a disorder of progressive memory loss and confusion in Frau Auguste Deter, a 46-year-old woman. After she died on 8 April 1906, he examined her brain and saw that it was full of unusual protein clumps known as plaques. Over a century later, we now know that these plaques are full of a protein called amyloid-beta (Aβ) and are one (out of four) hallmark(s) of the disease that bears Alzheimer's name (see Fymat, 2019h). While other features of AD have since been discovered, the theory that Aβ is the main cause of this so far incurable disease has unfortunately (and erroneously) long dominated the discourse.
There are many subtle variations of the "amyloid-beta hypothesis", but generally the theory goes that Aβ accumulates in the brain, then clumps together. Somewhere in this process, nerve cells in the brain become damaged, which leads to memory loss and other well-known symptoms of AD. So, it was thought, the approach to treating the disease should be rather straightforward – stopping the clumping would halt the disease!
Unfortunately, decades of research, many failed clinical trials later, and many billions of dollars in research spending by governments and the pharmaceutical industry (Roche Holding AG, Eli Lilly & Co., Eisai Co. and others), it appears that this approach is not working. The most recent plaque-busting treatment has been Aducanumab – an antibody-based therapy designed to stick to and destroy Aβ. Initial data suggested that the treatment did indeed clear Aβ from the brain. But the clinical trials, which involved thousands of patients, produced apparently disappointing results and were stopped by the drug company Biogen & Esai because they “...(the trials) were unlikely to meet their primary end-point upon completion". It is very hard to tell what is truly the situation without the full information (not available) from the Aducanumab trial. Some have ventured that may be the disease had progressed too far in the participants for the treatment to be effective. Perhaps also the small Aβ oligomers had already done their damage, setting the disease in motion before the participants were even recruited to the trial. Earlier trials with other Aβ-busting drugs had shown that, in some cases, the disease even worsened! Further, some people with large accumulations of plaques do not necessarily have symptoms of dementia.
This has led many to ask whether the amyloid hypothesis of AD should be abandoned. In reality, few neuroscientists still subscribe to the view that it is the Aβ plaques themselves that cause the symptoms of AD. Studies with mice that mimic human AD have shown that memory loss occurs “before” plaques form in the brain. Other studies have suggested that it is the smaller fragments (called "oligomers") of Aβ that are really toxic to nerve cells. And it has even been suggested that the formation of plaques is a manifestation of the brain rounding-up all these dangerous oligomers into one place for safety.
I believe that we got the cause of AD all wrong and we had been sidetracked for very long. Like in so many medical treatments, when we cannot find the root cause of the disease, we treat a surrogate end-point, which would be acceptable had the surrogate end-point been demonstrably shown to be uniquely correlated with the real end-point. Unfortunately, in many of those treatments, that correlation was not established. While we treat that surrogate, the disease continues along its devastating course, and so it has been with Alzheimer's. Clearing the plaques (the surrogate) did not cure AD (the real issue). It is therefore high time to think the disease anew, to identify its root cause, and to come up with a cure.
As a prelude to my theory regarding the root cause of AD, a brief introduction to the salient features of the human immune system would be helpful.
A Cursory Introduction to The Human Immune System
The human immune system is a host defense system that protects against disease. To function properly, it must detect a wide variety of agents known as pathogens (microbes, viruses, fungi, parasitic worms, etc.), distinguish them from the organism's healthy tissue, destroy or neutralize them, and keep a memory of them in case they further attack. The defense system is multi-layered and consists of physical, chemical, and biological defense layers of increasing specificity. (To utilize a military analogy, think about a multi-layered anti-ballistic missile defense system with built-in memories of the electronic “signatures” of incoming enemy missiles. That defense system can recognize the incoming missiles through their signatures and is capable of intercepting and destroying the missiles originating from different ranges. If new waves of missile attacks take place, through the stored memories, the system is again capable of intercepting and neutralizing or destroying them. However, if the incoming missiles are so numerous as to overwhelm the defense system, this system ceases operating, and the attack continues and spreads to an ever wider enemy terrain to the ultimate point of obliterating the enemy.)
The immune system is composed of two complementary and mutually cooperative components: the peripheral (body) component and the cerebral (brain) component. Each of these, in turn, includes two subsystems: the innate (also called humoral) immune subsystem and the adaptive (or acquired or cell-mediated) subsystem. Additionally, the brain protective barriers [which include the blood-brain barrier (BBB) proper, the blood-cerebrospinal fluid barrier (BCSFB), the retinal-brain barrier (RBB), and similar fluid–brain barriers] separate the peripheral regions of the immune system (which protect the body) from the internal neuroimmune system (which protects the brain). In brief, a number of known neurological and NDDs are mediated by a disruption or failure of the BBB. While understanding the nature of the barrier's role (and also the role of multi-drug resistance) is imperative in designing treatments, the fundamental question of whether the compromised integrity of the barrier is a component of the etiology of the disease under consideration or a consequence of it remains unanswered.
During an infection, the immune system adapts its response to improve its recognition of the pathogen (in much the same way as the illustrative anti-ballistic missile system selects from its memory those electronic signatures that best match the incoming missiles before firing). Antigens (short for antibody generators – the enemy missiles) are pathogens that elicit an immune response to counter them in the form of antibodies (the friendly missiles). There are approximately 400 known neurological diseases, some of which being classified as mental disorders. A number of these disorders are mediated by a disruption or failure of the BBB. Unfortunately, studies of this barrier within the context of clinical investigations have historically been limited. Nonetheless, in the case of AD, I initially posit that the compromised integrity of the barrier is a component of the etiology (cause) of the disease, not a consequence of it, allowing the intrusion of pathogens (microbes, viruses, fungi, etc.) in the brain.
The above varied barriers prevent pathogens from entering the organism. If a pathogen breaches the layered defense system or the brain protective barriers, the innate immune system provides an immediate, but non-specific response. If the pathogen successfully evades it, the adaptive immune system is activated. This improved response is retained even after the pathogen has been eliminated, in the form of an immunological memory. This memory property allows the adaptive immune system to mount faster and stronger attacks each time that pathogen is again encountered. (This is not very different from the old form of battle taking place between two enemy armies. When one army attempts to invade the territory of another, the latter sends in first a large number of countering battalions in a firehose-like fashion, attacking the enemy in many different fronts without any pinpointed tactic. If the enemy army is still able to withstand or evade that first assault, then other battalions are sent in with a more specifically targeted tactic.)
The Innate Immunity Subsystem Began at Conception
The immune system evolves and changes from conception to death. Thus, newborn infants have no prior exposure to antigens and are particularly vulnerable to infection. However, during pregnancy, the mother provides several layers of passive protection so that at birth the baby has high levels of antibodies with the same range of specificities as those of the mother. In addition, breast milk or colostrum transfers antibodies to the gut of the infant to protect it against bacterial infections until such time as the newborn can synthesize its own antibodies. All of the above represents passive immunity because the fetus does not actually make by itself any antibodies or memory cells that would remember previous attacks from the same antigens - it only borrows the mother's antibodies. This initial passive immunity is usually short-term, lasting from a few days up to several months at most until the baby is born. What remains of it after birth will evolve as the baby grows and develops into adulthood (it can be boosted even from one person to another by the use of an antibody-rich serum) and throughout its lifetime.
The Acquired Immunity Subsystem Began at Birth
A personal active immunity has likewise developed in parallel to the passive immunity although it started later at the moment of birth not at conception. After an initial response to a specific pathogen, this adaptive (or acquired) immunity additionally creates an immunological memory that leads to an enhanced response to subsequent encounters with the same pathogens. This process of acquired immunity is actually the basis of vaccination.
As we age, our immune system (both its innate and acquired subsystems) evolves and adapts while progressively losing some of its strength. It becomes compromised to different degrees depending on the individual, conferring a spectrum of different degrees of susceptibility to disease.
Now, the host immunity system evolves to echo the presence and evolution of pathogens which also adapt to avoid detection and neutralization. There is an almost inverse relationship between the level of integrity of the immune system and the level of proliferation of the pathogens. The more impaired is the immune system, the less pathogens can be neutralized. Table 1 contrasts the properties between the two subsystems.
| Innate Immune System | Acquired Immune System |
| Dominant system of host defense | Complementary system of host defense |
| Non-specific (generic) response to pathogens | Specific response to pathogens |
| Immediate maximal response to exposure | Lag time between exposure and maximal response |
| No immunological memory | Immunological memory |
| Ability to distinguish between healthy tissues and antigens | Ability to distinguish between healthy tissues and antigens |
| Can be artificially transferred from one individual to another via antibody-rich serum | Cannot be transferred |
Table 1: Components of the immune system
In the fight against AD, both the peripheral (body) and the cerebral (brain) immune components play an important role, not just the latter, as will be discussed below.
The Body's Immune System Plays a Larger Role in Ad Than Thought Previously
The microglia are specialized native immune cells that serve as the central nervous system (CNS)'s first lines of defense against infection and injury. They are present throughout the brain and spinal cord, are constantly monitoring their environment, and can be switched on or activated to perform different functions such as control inflammation, destroy pathogens, clean up the debris from dead or damaged cells, and seal off the site of an injury. However, in AD, the microglia appear to be fighting a losing battle.
While many studies have explored the role of microglia in AD, very few researchers have asked whether a different set of immune cells (the T- and B-cells that play a large part in autoimmune diseases outside the brain) might also impact Alzheimer's. Researchers at the University of California at Davis demonstrated just that with genetically-modified AD mice. They confirmed the importance of this interplay between immune cells in the blood and those in the brain.
Lastly, it is known that the immune system changes with age and becomes less capable of making T- and B-cells. So, might aging of the immune system in humans contribute to the development of AD? As I posited earlier, I believe so, and this is why AD affects mostly the older population (~ 90% of AD patients) whose immune system has become deficient or impaired as they aged.
But, not only does the body's immunity system help clear the amyloid-beta plaques in the brain so does the brain's immune system, as discussed next.
The Brain's Immune System Could Also Be Harnessed To Help Clear Plaques
In the past, owing to the presence of the brain's protective barriers (BPB) at the interface between the central nervous system and the periphery, and their muted response to neuroinflammation, it had been widely assumed heretofore that the brain (and, more generally, the CNS) is immune-privileged. However, in contrast to this earlier dogma, it is now evident that these immune capabilities do exist. The brain's vaguely understood component of the immune system is normally able to handle, treat, and overcome any adverse pathologies developing therein. It fails when the insult is so unsurmountable as to cause the immune system to go haywire. Despite the protective mechanisms of the barriers, the capacity for immune-surveillance of the brain is maintained, and there is evidence of inflammatory signaling at the brain barriers that may be an important part of the body's response to damage or infection. This signaling system appears to change both with normal aging and during disease.
A new study appearing in the Journal of Neuroinflammation (issue of April 2019) suggests that the brain's immune system could also potentially be harnessed to help clear the amyloid plaques. This confirms earlier observations that, when activated to fight inflammation, the brain's immune system also plays a role in the removal of Aβ. It can also be manipulated in a manner that accelerates the process. The researchers conducted a series of experiments on mouse models of AD to see if they could replicate the phenomenon of Aβ clearance absent brain inflammation. For this purpose, they "tricked" the microglia into action by injecting a specific protein molecule (a cytokine - a molecule that plays an important role in cell signaling) into the brain. They were able to replicate the mechanisms that instruct the microglia to activate an anti-inflammatory response and observed a more than 60% reduction in Aβ in the brain.
While much remains to be done to fully understand the complexity and potential unintended consequences of this approach, it is clear that microglia play an important role in the removal of Aβ from the brain. However, contrary to the researchers' conclusion, I do not believe that the microglia may lead to a “novel approach to treating this disease (i.e., AD)” for two main reasons: (1) Clearing the amyloid plaques does not treat (or contribute to treat) AD and further may, in certain cases, even worsen the disease; and (2) the amyloid plaques are not the root cause of the disease (only one of its symptoms) so that, in the absence of cause-and-effect, a cure will not ensue. Nonetheless, the above experiments are important in a different regard. They demonstrated that the brain immune system can be manipulated by cytokines or perhaps other molecules as well. Harnessing the brain immune system so it does not go rogue is part of what I am advocating.
The Brain's Immune System is an Ally, Not an Enemy, In The Battle Against AD
Because the microglia always surround the plaques, many have theorized that they are responsible for inflammation and damage to surrounding brain cells. However, that theory appears to be wrong, according to a new study by Yale School of Medicine researchers (see Nature Communications, 29 January 2019). Actually, rather than causing damage, the microglia seem to protect the brain by “corralling” the amyloid plaques. Since some people with large accumulations of plaques do not necessarily have symptoms of dementia, the scientists searched for other causes of cognitive decline and zeroed-in on inflammation. Unfortunately, Alzheimer's drugs that target inflammation in the brain have failed to show any benefit.
Using high-resolution imaging technology with mouse models of AD, the researchers have shown that, as we age, we lose microglia and become less able to confine plaques, leading to the release of plaque toxins that destroy the connections between neurons. Thus, microglia actually act as a physical barrier that slows the expansion of plaques and blocks the ability of free-floating Aβ proteins to bind to the plaques and cause toxicity.
In brief, by improving the microglia's shielding function, it is possible to reduce toxicity to neurons, which is another feature of my proposal.
Having cursorily reviewed the peripheral and brain immune systems and their interactions in the battle against AD, it is now time to discuss diseases resulting from disorders of the immune system.
Diseases Resulting From Disorders of The Immune System
The immune system is a remarkably effective structure that incorporates specificity, inducibility, and adaptation. Failures of host defense do occur, however, and fall into three broad categories: immunodeficiencies, autoimmunity, and hypersensitivities.
Immunodeficiencies
Immunodeficiency occurs when the immune system is less active than normal, resulting in recurring and life-threatening infections. This can either be the result of a genetic disease such as a severe combined immunodeficiency, or the use of immunosuppressive medication, or else acquired conditions such as HIV/AIDS.
Immunodeficiencies also occur when one or more of the components of the immune system are inactive. The ability of the immune system to respond to pathogens is then diminished in both the young and the elderly, with immune responses beginning to decline at around 50 years of age due immunosenescence. In developed countries, obesity, alcoholism, and drug use are common causes of poor immune function. However, malnutrition is the most common cause of immunodeficiency in developing countries. Diets lacking sufficient protein are associated with impaired cell-mediated immunity, complement activity, phagocyte function, IgA antibody concentrations, and cytokine production. Additionally, the loss of the thymus at an early age through genetic mutation or surgical removal results in severe immunodeficiency and a high susceptibility to infection. Immunodeficiencies can also be inherited or acquired. Chronic granulomatous disease, where phagocytes have a reduced ability to destroy pathogens, is an example of an inherited, or congenital immunodeficiency. AIDS and some types of cancer cause acquired immunodeficiency.
Autoimmunity
Disorders of the immune system can also result in autoimmune diseases but also inflammatory diseases and cancer. Autoimmune diseases result from a hyperactive immune system that attacks normal tissues as if they were foreign organisms. Common autoimmune diseases include Hashimoto's thyroiditis, rheumatoid arthritis, diabetes mellitus type 1, and systemic lupus erythematosus... and I posit neurodegenerative diseases including AD.
Overactive immune responses comprise the other end of immune dysfunction, particularly the autoimmune disorders. Here, the immune system fails to properly distinguish between its own molecules (called self molecules) and other molecules (called non-self molecules), and attacks part of the body. Under normal circumstances, many T-cells and antibodies react with self-peptides. One of the functions of specialized cells (located in the thymus and bone marrow) is to present young lymphocytes with self-antigens produced throughout the body and to eliminate those cells that recognize self-antigens, preventing autoimmunity.
Hypersensitivity
Hypersensitivity is an immune response that damages the body's own tissues. It is divided into four classes (Type I – IV) based on the mechanisms involved and the time course of the hypersensitive reaction:
- Type I hypersensitivity: is an immediate or anaphylactic reaction, often associated with allergy. Symptoms can range from mild discomfort to death. Type I hypersensitivity is mediated by IgE, which triggers degranulation of mast cells and basophils when cross-linked by antigen;
- Type II hypersensitivity: occurs when antibodies bind to antigens on the patient's own cells, marking them for destruction. This is also called antibody-dependent (or cytotoxic) hypersensitivity, and is mediated by IgG and IgM antibodies;
- Type III hypersensitivity: Immune complexes (aggregations of antigens, complement proteins, and IgG and IgM antibodies) deposited in various tissues trigger Type III hypersensitivity reactions; and
- Type IV hypersensitivity (also known as cell-mediated or delayed type hypersensitivity) usually takes between two and three days to develop. Type IV reactions are involved in many autoimmune and infectious diseases, but may also involve contact dermatitis (poison ivy). These reactions are mediated by T-cells, monocytes, and macrophages.
Idiopathic Inflammation
Inflammation is one of the first responses of the immune system to infection, but it can appear without known cause. Inflammation is produced by eicosanoids and cytokines, which are released by injured or infected cells. Eicosanoids include prostaglandins that produce fever and the dilation of blood vessels associated with inflammation, and leukotrienes that attract certain white blood cells leukocytes). Common cytokines include interleukins that are responsible for communication between white blood cells; chemokines that promote chemotaxis, an interferons that have anti-viral effects, such as shutting down protein synthesis in the host cell, and growth factors and protein synthesis in the host cell. Growth factors and cytotoxic factors may also be released. These cytokines and other chemicals recruit immune cells to the site of infection and promote healing of any damaged tissue following the removal of pathogens.
But, how has the immune system been manipulated in medical treatments?
Immune System Manipulations in Medicine
The immune response can be manipulated to suppress unwanted responses resulting from autoimmunity, allergy, and transplant rejection, and to stimulate protective responses against pathogens that largely elude the immune system or cancer. Manipulations include immunosuppression, immunostimulation, and vaccination. For AD, I am principally prescribing the combined use of immunosuppression and immunostimulation:
- Immunosuppression: Immunosuppressive drugs are used to control autoimmune disorders or inflammation when excessive tissue damage occurs, and to prevent transplant rejection after an organ transplant. In inflammation cases, anti-inflammatory drugs are often used to control them. Glucorticoids are the most powerful of these drugs; however, these drugs can have many undesirable side effects, such as central obesity, hyperglycemia, osteoporosis ... so their use must be tightly controlled. Lower doses of anti-inflammatory drugs are often used in conjunction with cytotoxic or immunosuppressive drugs such as Methotrexate or Azathioprine. Cytotoxic drugs inhibit the immune response by killing dividing cells such as activated T-cells. However, the killing is indiscriminate and other constantly dividing cells and their organs are affected, which causes toxic side effects. Immunosuppressive drugs such as Cyclosporin prevent T-cells from responding to signals correctly by inhibiting signal transduction pathways.
- Immunostimulation: Cancer immunotherapy covers the medical ways to stimulate the immune system to attack cancer tumors.
- Vaccination: Long-term active memory is acquired following infection by activation of B- and T-cells. Active immunity can also be generated artificially, through vaccination. The principle behind vaccination (also called immunization) is to introduce an antigen from a pathogen in order to stimulate the immune system and develop specific immunity against that particular pathogen without causing disease associated with that organism. This deliberate induction of an immune response is successful because it exploits the natural specificity of the immune system, as well as its inducibility. With infectious diseases remaining one of the leading causes of death in the human population, vaccination represents the most effective manipulation of the immune system mankind has developed. However, in as much as vaccines may over-stimulate the immune system, they will not be helpful in the case of AD with its over-active, runaway autoimmune system. They could, however, if the vaccines were devoid of adjuvants that enhance the immune system.
Most viral vaccines are based on live attenuated viruses, while many bacterial vaccines are based on acellular components of micro-organisms, including harmless toxin components. Since many antigens derived from acellular vaccines do not strongly induce the adaptive response, most bacterial vaccines are provided with additional adjuvants that activate the antigen-presenting cells of the innate immune system and maximize immunogenicity. In the case of AD, those additional adjuvants would have to be foregone.
Predicting Immunogenicity
Larger drugs (>500 Da) can provoke a neutralizing immune response, particularly if the drugs are administered repeatedly, or in larger doses. This limits the effectiveness of drugs based on larger peptides and proteins (which are typically larger than 6000 Da). In some cases, the drug itself is not immunogenic, but may be co-administered with an immunogenic compound, as is sometimes the case for Taxol. Computational methods have been developed to predict the immunogenicity of peptides and proteins, which are particularly useful in designing therapeutic antibodies, assessing likely virulence of mutations in viral coat particles, and validation of proposed peptide-based drug treatments. Early techniques relied mainly on the observation that hydrophylic amino acids are over-represented in epitope regions than hydrophobic amino acids; however, more recent developments rely on machine learning techniques using databases of existing known epitopes, usually on well-studied virus proteins, as a training set. A publicly accessible database has been established for the cataloguing of epitopes from pathogens known to be recognizable by B-cells. The emerging field of bioinformatics-based studies of immunogenicity is referred to as immunoinformatics. Immunoproteomics is the study of large sets of proteins (proteomics) involved in the immune response.
Can The Baffling Relationship of Age and AD be Explained By a Progressively Declining Immune System?
It is my contention that AD is a hyperactive autoimmune disorder that has run amok as we age and can no longer handle the levels of biological insults to which we are exposed. Since conception, we had in us the seeds of neurodegenerative diseases including AD. Depending on our age and the strength of our immune system, AD manifests itself at certain ages (early onset AD) and more particularly as we get older (late onset AD) in tune with the diminishing efficiency of our immune system. Thus, the age-old (no pun intended) dilemma can be explained immunologically.
On The Root Cause of Alzheimer's As a Conflict Resolution Issue
I have submitted in separate publications (Fymat, 2017-2021) that the root cause of Alzheimer's is the autoimmune system (both its peripheral and cerebral components) that had run amok (a sort of run- away effect) in its unsuccessful attempts to maintain brain homeostasis between promoting and destroying forces that act on the synapses. (In the military analogy, this is when the wave of attacking missiles has overwhelmed the anti-ballistic missile defense system.) In other words, it is a conflict resolution issue between the antagonistic synaptoblastic (promoting) and synaptoclastic (destroying) pressures. This balancing process consists of two phases:
- The synapse- building (or synaptoblastic) phase: Neurons sport receptors called amyloid precursor proteins (APP) that grab hold of netrin-1 (these are molecules floating by in the intercellular environment) and send signals to the neurons to keep them healthy and functional. When this process fails, the next phase takes place:
- The synapse-destroying (or synaptoclastic phase): It defaults to opposite signals that instruct the neurons to commit suicide and to the APPs to produce more Aβ, thereby outnumbering netrin-1. As a consequence, the APPs are less likely to grab netrin-1 and more likely to keep grabbing Aβ. Any effective treatment for Alzheimer's should therefore include a method to rebalance the synapse building and dismantling phases, not enhancing or destroying either phase.
The cure would therefore include a balancing of these opposing pressures by regulating the brain's immune system, neither fiercely combating the hyper-excited synaptoblastic pressures nor suppressing the depressing synaptoclastic ones.
Putative immunological therapies, based on the concept of training the immune system to recognize, attack, and reverse the deposition of Aβ have been designed. Unfortunately, as already stated earlier, such a surrogate end-point has not been clinically demonstrated to cure the disease, i.e., even after the amyloid plaques had been cleared, the disease symptoms persisted and the disease itself became worse in some circumstances and continued its deleterious progress. Further, people with extensive plaques may not have dementia. Still further, immunotherapeutic agents have been found to cause some concerning adverse drug reactions. In addition ,one important limitation of active and passive immunotherapy as currently practiced is the low amount of antibodies that can pass the BBB (this may, however, be overcome by coupling antibodies, the antigen fighters, to the peptide penetratin). In distinction with the antibodies employed, several small molecules have been designed to readily pass the barrier while delivering therapeutic compounds at the right locations in the right dosage amounts, heralding a new treatment approach. This is also what nanotechnology (NT) promises to do as nanoparticles (NPs) can be (and have been) designed to perform just such functions. However, while now well known, NT applications to NDDs has not yet been fully demonstrated.
A Path to a Cure for Alzheimer's
While palliative treatments are available, NDDs in general, and Alzheimer's in particular, have generally been declared as incurable. The reason is that we have not yet been able to identify the etiology and deep biology of their root cause(s). This situation is reminiscent of that for other diseases, particularly cancer. Thus, it may first be of interest to recall our past experience with immunotherapy as a cancer treatment.
Past Experience with Cancer
It was not until after we came to the realization that cancerous cells like healthy cells from which they evolve are braided in our genome, and that cancer is not an organ disease but the result of multiple genetic mutations, i.e., understanding the deep biology of cancer, that we have made great strides in cancer treatment and cure. Witness the emergence of immuno-oncology and the recent U.S. FDA-approved use of chimeric antigen receptor (CAR) T-cells to treat certain forms of melanoma.
Immunotherapy has been successful in inducing long-term remissions of hard-to-treat cancers. The early identified protein receptor on the surface of T-cells (the cytotoxic T-lymphocyte antigen 4, CTLA-4) and a molecule (named programmed death 1, PD-1) led to astonishing tumor shrinkage and increased survival, particularly in metastatic melanoma.
Thus, anti-CTL-4 cells and anti-PD-1 molecules have opened up new vistas in tumor treatment. Beyond that, genetically-modified patient's T-cells and PD-1 molecules promise to be even more effective in specifically tailoring the treatment to the patient along the precepts of personalized medicine.
Natural Immunotherapy with Natural Treg Cells
In parallel with immunotherapy as an emergent therapy of cancer, I advanced earlier the opinion that brain immunotherapy should also become a similar therapy for brain cancers and neurological disorders (Fymat, 2017d-h, 2018e-f), providing a paradigm shift in our therapeutic approach to brain cancer and these disorders.
The approach advocated here would be to regulate the underlying autoimmune system (not to either enhance it immeasurably or suppress it totally), to boost in a measured manner the synaptoclastic signals while at the same time taming down the synaptoblastic signals. This idea builds upon work done in diabetes type I, an incurable disease so far, in which the autoimmune system is taught to tolerate the insulin-producing cells of the pancreas so that it does not destroy the diabetic patient's ability to produce the glucose-regulating insulin. The similar idea forms the basis of various clinical trials for treating other incurable diseases such as multiple sclerosis and Graves' disease. The overarching purpose is to harness the hyperactive autoimmune system. This can be accomplished in two manners by:
- Employing naturally existing molecules: These can induce an immune response (antigens) or
- Employing engineered immune cells: These can train the autoimmune system to tolerate the process or tissue it is on track to damage.
The above idea has the potential to cure a range of autoimmune disorders, including especially neurological and neurodegenerative disorders, and particularly Alzheimer's. This requires a deep understanding of the molecular basis of autoimmunity, including brain and central nervous system immunity, as well as advances in genetic engineering and cell-based therapy. Caution must nonetheless be exercised as deploying the immune system to treat certain diseases can also potentially trigger other autoimmune diseases, e.g., in the case of cancer, it may additionally trigger rheumatoid arthritis and colitis.
The main immune players are the regulatory T-cells (Treg), which act as the brakes of the immune system. Similarly to other T-cells, Treg-cells rein in the immune cells that are doing damage. It has been suggested that the body can be made to produce the Treg-cells required to dampen a certain autoimmune response by dosing people who are affected with the same antigen or antigens that the immune system wrongly interprets as a reason to attack. This was tested for multiple sclerosis, demonstrating less brain inflammation. The approach is similar to vaccination without the immune-system stimulants called adjuvants that are usually included in vaccine formulations. Here, antigens can induce a calming effect through Treg-cells.
Synthetic Immunotherapy with Engineered Treg Cells
There may be other ways to temper a rogue autoimmune system. For example, in cell-based therapy, a patient's Treg-cells can be removed from the body, engineered to respond to specific antigens that have been wrongly recognized by the immune system as being foreign, and then returned to the body. This is the very principle of the FDA-approved chimeric antigen receptor (CAR) T-cells (here Treg-cells) that have been applied to cancer treatment.
Stem Cell Therapy
Stem cell therapy is the use of stem cells (SC) to treat or prevent a disease or condition. One of the oldest form of it is bone marrow transplantation that has been used for many years without controversy. To appreciate the advantages and disadvantages of this other form of therapy, and its potential application for the treatment of NDDs including AD and ultimately dementia, I provide an introduction to stem cells in the Appendix. Of particular interest to us are regenerative treatments, and the treatment of neurodegenerative conditions.
In regenerative treatment, SCs mediate repair via five primary mechanisms:
- Providing an anti-inflammatory effect;
- Homing-in onto damaged tissues and recruiting other cells (usually, endothelial progenitor cells that are necessary for tissue growth);
- Supporting tissue remodeling over scar formation;
- Inhibiting apoptosis (or cell death); and
- Differentiating into bone, cartilage, tendon, and ligament tissue.
To further enrich blood supply to the damaged areas, and consequently promote tissue regeneration, platelet-rich plasma could additionally be used in conjunction with the therapy. The efficacy of some SC populations may be affected by the method of delivery.
The advantages of SC therapy include: lessening the symptoms or conditions of the disease treated and allowing patients to reduce their drug intake.
In the case of neurodegeneration and neurodegenerative diseases, it is known that healthy adult brains contain neural SCs, which divide to maintain general stem cell numbers, or become progenitor cells. In healthy laboratory animals, progenitor cells migrate within the brain and function primarily to maintain neuron populations for olfaction (the sense of smell). In these animals, research has been conducted on the effects of SCs on brain degeneration including such brain diseases as AD, Parkinson's disease (PD), amyotrophic lateral sclerosis (ALS - also known as Lou Gehrig's disease), and multiple sclerosis (MS). Of particular note, pharmacological activation of endogenous neural SCs has been reported to induce neuroprotection and behavioral recovery in adult rat models of neurological disorder.
There are, unfortunately, several potential disadvantages: In the case of cancer, the treatment may require immunosuppression before transplantation,; this is in order to perform a preliminary radiation treatment to kill previous cancerous cells or because the patient's immune system may target the SCs considering them as foreign bodies (but this could be avoided using SCs from the same patient); pluripotency in certain SCs could make it difficult to obtain a specific cell type; not all cells in a population differentiate uniformly, making it difficult to obtain the exact cell type needed; undifferentiated cells can create tissues other than the desired types; and pluripotent stem cells (PSC) can form tumors, which is particularly the case for embryonic, fetal, and induced PSCs.
In the case of neurodegenerative diseases, including especially AD and dementia, SCs have been shown to have a low immunogenicity (the promotion of immune properties) due to the relatively low number of major histocompatibility complex (MHC) molecules found on their surface. They have also been found to secrete chemokines that alter the immune response and promote tolerance of the new tissue. Notwithstanding this low immunogenicity of SCs, I would still advocate SC therapy for the treatment of Alzheimer's and dementia only under the following conditions: A prior radiation treatment is not required so as not to suppress the immune system, minimizing the secretion of chemokines so as not to adversely alter the immune response, and minimizing if not eliminating any possibility of inducing cancer.
Use of Palliative Therapeutic Aids
Several palliative aids have been recommended as discussed in my earlier publications. In particular, the immune system is affected by sleep and rest, with sleep deprivation being detrimental to immune function. When suffering from sleep deprivation, active immunization may have a diminished effect and may result in lower antibody production so that a lower immune response would be noted than in a well-rested individual. In addition to the negative consequences of sleep deprivation, sleep and the intertwined circadian system have been shown to have strong regulatory effects on immunological functions, affecting both the innate and the adaptive immunity. In addition, the decrease in hormone production is also thought to adversely affect the formation of long-lasting immune memory while eliciting a less than effective response against any intruding pathogens.
Like in other diseases (diabetes, cancer, etc.), we have been hampered by our imperfect understanding of the underlying biology and, in desperation, have too soon declared such diseases as incurable. However, the realization that the brain and the CNS are endowed with their own immune system, accompanied by the greater understanding of the mechanism of autoimmunity, and the advent of cell-based therapy will empower us to conceive other treatment strategies and even cures as I have attempted to do here in the case of Alzheimer's. The main immune players, the regulatory T-cells (Treg), which act as the brakes of the immune system, can be so manipulated (engineered) as to temper and regulate the autoimmune system and train it to tolerate (rather than fiercely combat) the opposing pressures to achieve brain homeostasis. There may also be additional ways to temper a rogue autoimmune system such as, for example, emulating cancer immunotherapy with CAR-T cells but with CAR-Treg cells for the neurodegenerative diseases of interest. Stem cell therapy could also be considered provided certain conditions are met: no prior radiation treatment, minimization/elimination of the secretion of chemokines, and minimization/elimination of any possibility of inducing cancer.
Conclusions
- For the past century, we got the cause of Alzheimer's all wrong. The amyloid-beta plaques and other hallmarks of the disease are not the root cause of the disease but symptoms of it. We must now redirect our efforts.
- Microglia, the brain's resident immune cells, play an important role in the removal of amyloid- beta from the brain. The brain's immune system could be manipulated by cytokines or perhaps other molecules so it does not go rogue.
- The microglia always surround plaques but are not responsible for inflammation. Instead of causing damage, they protect the brain by corralling the plaques so that by improving microglia's shielding function, it is possible to reduce toxicity to neurons.
- Because some people with large accumulations of plaques do not necessarily have symptoms of dementia, other causes of cognitive decline must be at play. Inflammation is not one of them. Drugs that target inflammation in the brain have failed to show any benefit.
- As we age, we lose microglia and become less able to confine plaques, leading to the release of plaque toxins that destroy the connections between neurons. Thus, microglia actually act as a physical barrier that slows the expansion of plaques and blocks the ability of free-floating beta-amyloid proteins to bind to the plaques and cause toxicity. By improving that function, it is possible to reduce toxicity to neurons.
- The body's immune system with its three key cell types (T-, B-, and NK-cells) may play a larger part than anticipated in autoimmune diseases and also impact Alzheimer's. The loss of these immune cells increases amyloid-beta. The association of these three cell types with the microglia helps increase the clearance of amyloid-beta.
- The immune system changes with age and becomes less capable of making T- and B-cells, contributing to the development of Alzheimer's disease. This is why the disease affects mostly the older population (~ 90% of Alzheimer patients) whose immune system has become deficient or impaired as they aged.
- Natural or synthetic immunotherapy could be used taking advantage of experience acquired in the treatment of cancer with chimeric antigen receptor (CAR) T-cells and programmed cell death that have led to astonishing tumor shrinkage and increased survival, particularly in metastatic melanoma.
- Stem cell therapy could be contemplated provided only there is no prior radiation treatment so as not to suppress the immune system, the secretion of chemokines is minimized/eliminated so as not to adversely alter the immune response, and any possibilities of inducing cancer are minimized/eliminated.
- Pending full development of a cure, several palliative aids could be employed, including particularly measures to counter sleep deprivation that is detrimental to immune function.
Appendix
A Brief Introduction to Stem Cells
Stem cells are cells that can differentiate into other cell types and renew themselves by dividing and producing more of them. There are three broad types:
- Embryonic: They are formed prior to implantation in the uterus, 4-5 days after fertilization. They are pluripotent (see below) and can develop into each of the more than 200 cell types of the adult body. They continuously divide and become more specialized. Due to ethical considerations, many nations (including the U.S.) have moratoria or limitations on either research or production of new human embryonic stem cell lines. Nonetheless, because of their important properties, they remain a theoretically potential source for regenerative medicine and tissue replacement after injury or disease. In a developing embryo, the cells can differentiate into all the specialized cells (ectoderm, endoderm, mesoderm) and can maintain the normal turnover of regenerative organs (blood, skin, intestinal tissues, etc.).
- Fetal: There are two types: proper fetal which come from fetal tissue and are generally obtained after an abortion. They are not immortal but have a high level of division and are multipotent (see below); and extraembryonic from extra-embryonic membranes. They are usually not distinguished from adult stem cells.
- Adult: Also called somatic stem cells, they can also be found in children maintaining and repairing the tissue in which they are found. They have been successfully utilized for many years to treat leukemia and related bone/blood cancers. They are deemed multipotent (see below). In an adult organism, together with progenitor cells, the cells replenish tissues, acting as a repair system for the body. Progenitor and non-stem cells cannot self-renew. Adult stem cells are frequently used in various medical therapies.
Stem cells are endowed with two important properties: self-renewal and potency. The former property allows them to go through numerous cell division cycles while maintaining their own undifferentiated state. The latter property enables them to differentiate into specialized cell types. We distinguish four types of potency: totipotency (or omnipotency), that is, the cells are formed by the fusion of an egg and a sperm, can subsequently differentiate into embryonic and extra-embryonic cell types, and can construct a complete and viable organism. The second type, pluripotency, refers to stem cells derived from any of the three germ layers (endoderm, ectoderm, mesoderm) that can differentiate into a number of cell types, but only those of a closely related family of cells. The third type, oligopotency, refers to cells than can differentiate only into a few cell types. The fourth and last type, unipotency, refers to cells that can produce only their own type but can renew themselves.
Figure 1 is a pictorial showing diseases and conditions where stem cell treatment is promising or emerging.
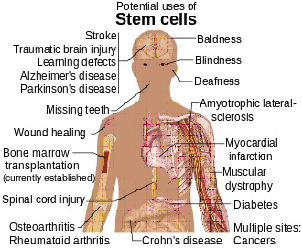
Source: Haggstrom Mickail, 2014
Figure 1: Diseases and conditions where stem cell treatment is promising or emerging.
(Not mentioned in Figure 1 are male infertility when due to absence of spermatogonial stem cells and female infertility including premature ovarian insufficiency.) Research is also underway in organogenesis (the formation of organs) in order to better understand human development and modeling human diseases.
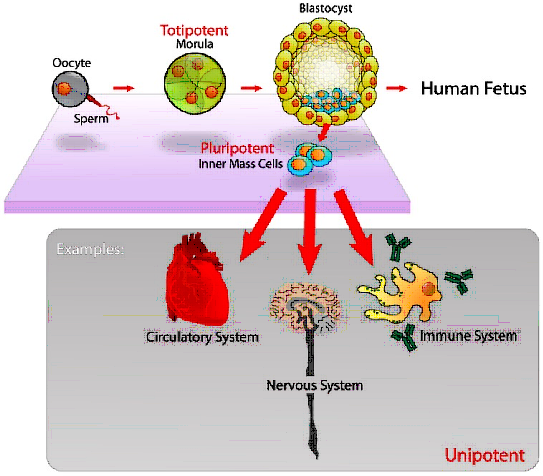
Source: Mike Jones (from the English Wikipedia)
Figure 2: Evolution from a fertilized egg to a human fetus and examples of transformation of inner mast cells in the circulatory, nervous, and immune systems.
It is possible to genetically reprogram adult stem cells that are multipotent into induced pluripotent stem cells that share many similar properties with embryonic stem cells (pluripotency, differentiation potential, expression of pluripotency genes, epigenetic patterns, etc.) but with many differences. They are viable and offer several therapeutic advantages such as especially to be able to create patient-specific pluripotent stem cells, which can be used in screening for side effects before drug treatment, as well as reducing risk of transplantation rejection.
Figure 2 illustrates the transformation from a fertilized egg to a human fetus and provides examples of the inner mass cells evolution into the circulatory, nervous and, importantly, immune system.
By a procedure called somatic cell nuclear transfer, stem cells can now be artificially grown and transformed (differentiated) into specialized cell types with characteristics consistent with cells of various tissues (muscles, nerves, etc.). This procedure is now preferred to that (described above) of inducing pluripotent stem cells.
There are four known accessible sources of autologous stem cells (that is, where the recipient and the donor are the same) that offer the least risk for harvesting:
- Bone marrow: Typically from the femur or the iliac crest, it is a rich source that is used for treating such conditions as liver cirrhosis, chronic limb ischemia, end-stage heart failure, etc.
- Adipose tissue: Fat cells obtained by liposuction.
- Blood: They are extracted by a procedure called apheresis wherein blood is drawn from the donor, passed through a centrifuge to extract the stem cells and the other blood components are returned to the donor.
- Umbilical cord blood: Usually preserved for the baby from whom the cells were extracted. They are stored in a “bank” to serve eventually later in case of a surgical or other emergency procedure.
- Amniotic fluid: These cells are very active, expand extensively without feeders and do not cause tumors. They are multipotent and can differentiate in cells of adipogenic, osteogenic, myogenic, endothelial, hepatic and also neuronal lines. They can be collected for autologous use.
- Skin: Now used in several applications, including in the treatment of multiple sclerosis.
References
- Alain L Fymat. “Alzheimer’s Disease: A Review”. Current Opinions in Neurological Science 2.2 (2018): 415-436. ISSN: 2575-5447.
- Alain L Fymat. “Neurological Disorders and the Blood Brain Barrier: 1. Epilepsy”. Current Opinions in Neurological Science 1.6 (2017): 277-293. ISSN: 2575-5447.
- Alain L Fymat. “Neurological Disorders and the Blood Brain Barrier: 2. Parkinson and Other Movement Disorders”. Current Opinions in Neurological Science 2.1 (2018): 362-383. ISSN:2575-5447.
- A.L. Fymat. “Immunotherapy: An Emergent Anti-Cancer Strategy”. Journal of Cancer Prevention & Current Research (Editorial) 7.3 (2017):1-4.
- A.L. Fymat. “Synthetic Immunotherapy with Chimeric Antigen Receptors”. Journal of Cancer Prevention & Current Research 7.5 (2017):1-3.
- A.L. Fymat. “Immunotherapy of Brain Cancers and Neurological Disorders”. Journal of Cancer Prevention & Current Research 8.6 (2017):1-7.
- Alain L Fymat. “Immuno-Therapy: A New Frontier in Cancer Care”. Holistic Approaches in Oncotherapy 1.1 (2017): 8-13.
- A.L. Fymat. “Cancer Therapy with Chimeric Antigen Receptors – A Landmark Moment for Cancer Immunotherapy”. Journal of Cancer Prevention & Current Research 8.6 (2017):1-7.
- A.L. Fymat. “Nanoneurology: Drug Delivery Across the Brain Protective Barriers”. Journal of Nanomedicine Research 5.1 (2017): 1-4.
- A.L. Fymat. “Therapeutics Delivery Behind, Through and Beyond the Blood Brain Barrier”. Open Access Journal of Surgery 5.1 (2017): 1-9.
- Alain L Fymat. “Blood Brain Barrier Permeability and Neurodegenerative Diseases”. Current Opinions in Neurological Science 2.2 (2018): 411-414. ISSN: 2575-5447.
- Alain L Fymat. “Regulating the Brain Autoimmune System: The End of All Neurodegenerative Diseases?” Current Opinions in Neurological Science 2.3 (2018): 475-479. ISSN:2575-5447.
- A.L. Fymat. “Roles of Nanomedicine in Clinical Neuroscience”. Global Journal of Nanomedicine 4.1 (2018): 13-15.
- A.L. Fymat. “Alzheimer's Disease: Prevention, Delay, Minimization and Reversal”. Journal of Clinical Research in Neurology 1.1 (2018): 1-16.
- Alain L Fymat. “Innate Immunotherapy of Recurring Glioblastomas: Preliminary Trials with Neutrophils”. Current Opinions in Neurological Science 2.3 (2018): 480-482. ISSN: 2575-5447.
- A.L. Fymat. “Harnessing the Immune System to Treat Cancers and Neurodegenerative Diseases”. Journal of Clinical Research in Neurology 1.1 (2018): 1-14.
- A.L. Fymat. “Is Alzheimer's an Autoimmune Disease Gone Rogue”. Journal of Clinical Research in Neurolog 2.1 (2018): 1-4.
- Alain L. Fymat. “Dementia Treatment: Where Do We Stand?” Current Opinions in Neurological Science 3.1 (2018): 599-603. ISSN: 2575-5447.
- A.L. Fymat. “On Dementia and Other Cognitive Disorders”. Journal of Clinical Research in Neurology 2.1 (2018): 1-14.
- A.L. Fymat. “Nanomedicine May Provide New Hope for Brain Cancer Therapy”. Global Journal of Nanomedicine 4.5 (2018): 1-7.
- A.L. Fymat. “Is Alzheimer's a Runaway Autoimmune Disease? And How to Cure It?” Proceedings of the European Union Academy of Sciences, Newsletter (2018): 379-383.
- AL. Fymat. “Dementia: A Review”. Journal of Clinical Psychiatry and Neuroscience 1.3 (2019): 27-34.
- Alain L Fymat. “Dementia with Lewy Bodies: A Review”. Current Opinions in Neurological Science 4.1 (2019): 15-32. ISSN: 2575-5447.
- A.L. Fymat. “What do we Know about Lewy Body Dementias?” Journal of Psychiatry and Psychotherapy (Editorial) 2.1 (2019): 1-4.
- Alain L Fymat. “The Pathogenic Brain”. Current Opinions in Neurological Science 3.2 (2019): 669-671. ISSN: 2575-5447.
- A.L. Fymat. “On the Pathogenic Hypothesis of Neurodegenerative Diseases”. Journal of Clinical Research in Neurology 2.1 (2019): 1-7.
- A.L. Fymat. “Electromagnetic Therapy for Neurological and Neurodegenerative Diseases: I. Peripheral Brain Stimulations”. Open Access Journal of Neurology and Neurosurgery 12.2 (2019): 30-47.
- A.L. Fymat. “Viruses in the Brain...? Any Connections to Parkinson's and other Neurodegenerative Diseases?” Proceedings of the European Union Academy of Sciences, Newsletter (2019): 249-252.
- A.L.Fymat. “Alzhei … Who? Demystifying the Disease and What You Can Do About it”. Tellwell Talent Publishers (2019): 236. ISBN: 978-0-2288-2420-6.
- Alain L. Fymat. “Recent Research Developments in Parkinson's Disease”. Current Opinions in Neurological Science 5.1 (2020): 12-30. ISSN: 2575-5447.
- A.L. Fymat. “Neuroradiology and its Role in Neurodegenerative Diseases”. Journal of Radiology and Imaging Science 1.1 (2020):1-14. Journal closed and transferred to: Journal of Neuroradiology and Nanomedicine 5(1):1-14.
- A.L. Fymat. “Electromagnetic Therapy for Neurological and Neurodegenerative Diseases: II. Deep Brain Stimulation”. Open Access Journal of Neurology and Neurosurgery 13.1 (2020): 1-17.
- AL. Fymat. “Nanobiotechnology-based Drugs for the Treatment of Neurological Disorders”. Journal of Pharmaceutical Bioprocessing 8.3 (2020): 1-3.
- A.L. Fymat. “Is Alzheimer's an Autoimmune Disease Gone Rogue? The Role of Brain Immunotherapy”. Journal of Clinical Research in Neurology 3.2 (2020): 1-3.
- A.L. Fymat. “Alzheimer's: What do we Know about the Disease and What Can Be Done About It?”. EC Journal of Psychology & Psychiatry 9.11 (2020): 69-74.
- A.L. Fymat. “Alzheimer's: Will there ever be a Cure?” Journal of Clinical Psychiatry and Neuroscience 3.4 (2020): 1-5.
- A.L, Fymat. “Parkinson's: What is Known about the Disease and What Can Be Done About It?” Journal of Clinical Research in Neurology 3.2 (2020): 1-12.
- A.L. Fymat. “Dementia: Should we Reorient our Approach to Treatment?”. EC Journal of Psychology & Psychiatry 9.12 (2020): 1-3.
- A.L. Fymat. “Dementia – What is its Causal Etiology?” International Journal of Neuropsychology and Behavioral Sciences 1.1 (2020): 19-22.
- A.L. Fymat. “Parkin... ss..oo..nn: Elucidating the Disease... and What You Can Do About it”. Tellwell Talent Publishers (2020): 258. ISBN: 978-0-2288-2874-7.
- A.L. Fymat. “Dementia: Fending off the Menacing Disease... and What You Can Do About it”. Tellwell Talent Publishers (2020): 488. ISBN: 978-0-2288-4145-3.
- A.L. Fymat. “Cancer Treatment: From Immunotherapy to Gene Therapy and Beyond”. Cancer Therapy & Oncology International Journal (Editorial) 18.2 (2021): 1-3.
- A.L. Fymat. “On Potentially Reversible Forms of Dementia”. Journal of Current Opinions in Neurological Science 6.1 (2021): 101-108.
- A.L. Fymat. “Dementia – Eliminating its Potentially Reversible Forms, Proc”. European Union Academy of Sciences (2021): 270-277.
- M. Schhwartz with A. London. “Neuroimmunity – A New Science that will Revolutionize how we Keep ou Brains Healthy and Young”. Yale University Press (2015): 283. ISBN: 978-0-300-20347.9.
Citation: Alain L. Fymat. “Alzheimer’s Disease: A Path To a Cure” Current Opinions in Neurological Science 7.1 (2022): 01-16.
Copyright: © 2022 Alain L. Fymat. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.