Research Article
Volume 2 Issue 6 - 2018
Incidence of Delayed Intracranial Hemorrhage in Patients Taking Warfarin that Sustain Head Trauma
Aria Jefferson Health, Department of Emergency Medicine, Philadelphia, PA, United States
*Corresponding Author: Maricel Dela Cruz DO, Aria Jefferson Health, Department of Emergency Medicine, Philadelphia, PA, United States.
Received: September 28, 2018; Published: October 05, 2018
Introduction
With an aging United States population, individuals taking anticoagulant medications, specifically warfarin are common. A large proportion of the elderly and those in lower socioeconomic classes utilize warfarin due to its affordability [1,2]. Emergency medicine physicians are challenged in treating these patients after they sustain head trauma [3,4]. It is agreed that the overall mortality in anticoagulated patients is significantly higher in patients on warfarin versus non-anticoagulated patients [5-9]. Of particular interest is the incidence of delayed intracranial hemorrhage in patients with blunt head trauma while on warfarin. To date, there is limited data on this matter.
Objectives
The objective of this study was to determine the incidence of delayed intracranial hemorrhage by computed tomography in individuals taking warfarin. It is hypothesized that the incidence of delayed intracranial hemorrhage in this specific population is low. As a result, this data can potentially prevent unnecessary admissions to the hospital, decrease radiation exposure, and reduce costs.
Materials and Methods
A retrospective observational study was conducted using the following software: Well soft ED charts, all scripts Sunrise inpatient data and radiographic studies on PACS from January 2009 to January 2012 at a Level II community trauma center, Aria Health Torres dale in Philadelphia, Pennsylvania. The Aria Health IRB approved this study. Participants included individuals admitted to the trauma services that were taking warfarin, suffered blunt head trauma, and had an in initially negative CT brain. Patient has to be 18 years or older to be eligible. There were no interventions performed, as this was a retrospective analysis.
Results
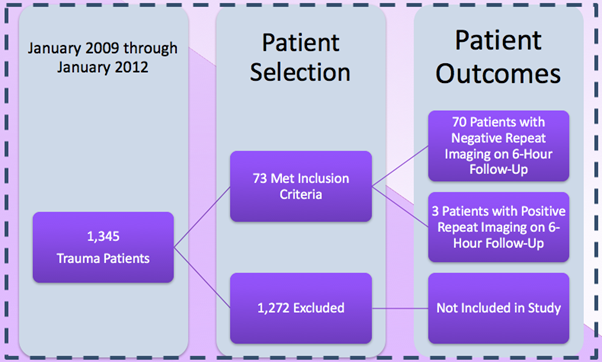
The primary outcome of this study was to determine the incidence of delayed intracranial hemorrhage in patients sustaining blunt head trauma while anticoagulated on warfarin from 2009 to 2012. In this chart review study, there were several thousand patients admitted to the trauma service during the time span of interest. Of those, 73 patients were admitted to the trauma service that satisfied this study’s inclusion criterion (See Figure). There were a multitude of blunt traumatic mechanisms of injury, including but not limited to: accidental falls, syncope, assaults, and motor vehicle collisions.
These patients were anti coagulated on warfarin for a variety of reasons, most commonly for atrial fibrillation. In this cohort, there were three patients who had an initially negative CT Brain that then developed an intracranial hemorrhage as demonstrated upon a 6-hour follow-up CT scan. The remaining 70 patients had negative imaging on a 6-hour follow-up CT Brain.
Conclusion
There is a risk of delayed intracranial hemorrhage in individuals using warfarin. This study found that none of the three patients with delayed intracranial hemorrhage had a significant change in their clinical status. No neurosurgical intervention was required. While there is a slight risk of delayed hemorrhage in this patient population, the most appropriate management may be to monitor these patients for clinical status change and only then could the decision for repeat imaging be made. On a systems-wide scale, this has the potential to decrease spending on imaging and reduce unnecessary radiation exposure.
References
- Franko J., et al. “Advanced age and preinjury warfarin anticoagulation increase the risk of mortality after head trauma”. The Journal of Trauma Injury, Infection, and Critical Care 61.1 (2006): 107-110.
- McMillian WD and Rogers FB. “Management of prehospital antiplatelet and anticoagulant therapy in traumatic head injury: a review”. The Journal of Trauma Injury, Infection, and Critical Care 66.3 (2009): 942-950.
- Brewer ES., et al. “Incidence and predictors of intracranial hemorrhage after minor head trauma in patients taking anticoagulant and antiplatelet medication”. The Journal of Trauma Injury, Infection, and Critical Care 70.5 (2011): E1-E5
- Claudia C., et al. “Minor head injury in warfarinized patients: indicators of risk for intracranial hemorrhage. The Journal of Trauma Injury, Infection, and Critical Care 70.4 (2011): 906-909.
- Cohen D.B., et al. “Traumatic brain injury in anti-coagulated patients”. The Journal of Trauma and Acute Care Surgery 60.3 (2006): 553-557.
- Hill J. “Delayed intracranial hemorrhage in the anticoagulated blunt trauma patient: routine repeat head computed tomography is unnecessary” Critical Care Medicine 41.12 (2013).
- Howard JL., et al. “Preinjury warfarin worsens outcome in elderly patients who fall from standing”. The Journal of Trauma and Acute Care Surgery 66.6 (2009): 1518-1522.
- Ivascu FA., et al. “Treatment of trauma patients with intracranial hemorrhage on preinjury warfarin”. The Journal of Trauma and Acute Care Surgery 61.2 (2006): 318-321.
- Joseph B., et al. “Repeat head computed tomography in anti-coagulated traumatic brain injury patients: still warranted”. The American Surgeon 80.1 (2014): 43-47.
- Nishijima DK., et al. “Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and pre-injury warfarin or Clopidogrel use”. Annals of Emergency Medicine 59.6 (2012):460-468
Citation:
Maricel Dela Cruz DO., et al. “Incidence of Delayed Intracranial Hemorrhage in Patients Taking Warfarin that Sustain Head
Trauma”. Current Opinions in Neurological Science 2.6 (2018): 591-593.
Copyright: © 2018Maricel Dela Cruz DO., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.