Research Article
Volume 1 Issue 6 - 2017
Downbeating Nystagmus in Benign Paroxysmal Positional Vertigo: an Apogeotropic Variant of Posterior Semicircular Canal
1Department of Neuro-Otology, Fundación San Lucas para la Neurociencia, Rosario, Argentina
2Department of Neuro-otology. INEBA (Instituto de Neurociencias de Buenos Aires), Argentina
3Otolaryngology Department, Hospital San Juan de Dios, University of Chile, Santiago, Chile
4Head of the division of ENT and Head and Neck Surgery, Hospital “Giovanni Paolo II”, Policoro, Italia
2Department of Neuro-otology. INEBA (Instituto de Neurociencias de Buenos Aires), Argentina
3Otolaryngology Department, Hospital San Juan de Dios, University of Chile, Santiago, Chile
4Head of the division of ENT and Head and Neck Surgery, Hospital “Giovanni Paolo II”, Policoro, Italia
*Corresponding Author: Sergio Carmona, Department of Neuro-Otology, Fundación San Lucas para la Neurociencia, Sarmiento 1501, Rosario, Santa Fe, Argentina.
Received: December 09, 2017; Published: December 13, 2017
Abstract
BPPV is the most frequent peripheral vestibular syndrome. In most cases, the interpretation of paroxysmal positional nystagmus presents no difficulty. We present a series of cases of patients with BPPV of posterior semicircular canal apogeotropic variant, atypical manifestation for this type of disorder. We included 20 patients who presenting symptoms and vestibular signs consistent with BPPV of the anterior canal and that, subsequently, were diagnosed as having PSC BPPV.
Keywords: Down beating nystagmus; Apogeotropic variant; Benign paroxysmal positional vertigo; Episodic vestibular syndrome; BPPV
Abbreviations: ASC: Anterior semicircular canal; BPPV: Benign paroxysmal positional vertigo; DB: Downbeating nystagmus; DH: Dix-Hallpike maneouver; LPSC: Left posterior semicircular canal; MRI: Magnetic resonance imaging; PPN: Paroxysmal positional nystagmus; PSC: Posterior semicircular canal; RPSC: Right posterior semicircular canal
Introduction
Benign paroxysmal positional vertigo (BPPV) is the most frequent within peripheral vestibular syndromes [1]. The interpretation, in most cases, of paroxysmal positional nystagmus (PPN) does not cause problems. The nystagmus typical of posterior semicircular canal (PSC) involvement due to canalolithiasis is vertical upwards (upbeating) with a torsional component towards the ear that is downward, so it can be considered as geotropic, also having the typical latency and with a duration of less than 1 minute [2-4]
Some patients who consult for positional vertigo, find a vertically down beating paroxysmal nystagmus with or without a clear torsional component, suggestive of BPPV due to anterior semicircular canal involvement (ASC), but which do not resolve with the maneuvers destined for that canal or that later develop a nystagmus with characteristics compatible with PSC BPPV, a behavior already described on another occasion by Vanucchi., et al. [1] We present a series of cases of patients with BPPV of posterior semicircular canal apogeotropic variant, atypical manifestation for this type of disease but that should be considered for the therapeutic and prognostic implications
Materials and Methods
We included 20 patients who consulted between January 2016 and April 2017, presenting symptoms and vestibular signs consistent with BPPV of the anterior canal and that did not resolve with replacement maneuvers for that canal. All the patients were evaluated by neurologists or otorhinolaryngologists with special dedication in neuro-otology. Neuroimaging was performed when it was considered necessary. These patients, subsequently, were diagnosed as having PSC BPPV, taking as a criterion the lack of response to the replacement maneuvers for ASC BPPV and the resolution of symptoms/signs with maneuvers for PSC (Semont and Epley).
Results
55% of the patients were women. The average age was 59.6 years. 17 patients consulted for vertigo/positional dizziness, and 8 patients complained of instability. 20% had a history of PSC BPPV, 2 patients with recurrent BPPV, and one patient with mild cranial trauma. 50% of the patients presented positional downbeat nystagmus without a torsional component. 55% of the patients underwent neuroimaging (MRI), which were normal.
All patients underwent replacement maneuvers for ASC BPPV, without obtaining successful results. 5 patients, in the control, develop signs of PSC BPPV. All the patients resolved their symptoms with maneuvers for PSC BPPV (Semont and Epley). (See Table 1) (See Video 1)
| No. | Sex | Age (years) | History | Reason for consultation | Physical examination | Neuroimaging | PSC BPPV maneuvers and results |
| 1 | M | 55 | Positional vertigo | DB positional nystagmus torsional left in right DH | None | Reverse Semont face down left, face up right, conversion to right posterior geotropic BPPV, resolve with right Semont | |
| 2 | M | 66 | Positional Dizziness and instability | DB positional nystagmus, torsional left in right DH | Normal | Epley for right PSC BPPV with improvement | |
| 3 | M | 74 | recurrent BPPV | Positional vertigo | DB positional nystagmus, torsional left in right DH | Normal | Epley for Right PSC BPPV with improvement |
| 4 | M | 45 | Positional vertigo | DB positional nystagmus torsional right in left DH | None | Reverse Semont face down right, face up left, conversion to left posterior geotropic BPPV, resolve with left Epley | |
| 5 | M | 34 | Head minor trauma | Positional vertigo and instability. | DB positional nystagmus torsional right in left DH | None | Epley for left PSC BPPV with improvement |
| 6 | F | 61 | Positional vertigo | DB positional nystagmus, torsional left in right DH | None | Epley for Right PSC BPPV, doesn’t resolve, Semont for right PSC BPPV with improvement | |
| 7 | F | 47 | Previous PSC BPPV | Positional vertigo | DB positional nystagmus, torsional left in right DH | Normal | Epley for Right PSC BPPV with improvement |
| 8 | F | 53 | Positional vertigo and instability | DB positional nystagmus torsional right in left DH | Normal | Epley for left PSC BPPV no improvement, resolve with Semont for left PSC BPPV | |
| 9 | F | 57 | Positional vertigo | DB positional nystagmus torsional right in left DH | Normal | Epley for left PSC BPPV with improvement | |
| 10 | F | 81 | Recurrent BPPV | Positional vertigo and dizziness | DB positional nystagmus, torsional left in right DH | Normal | Epley plus Semont for Right PSC BPPV with improvement |
| 11 | M | 70 | RPSC BPPV | Positional vertigo | DB nystagmus with no response to ASC repositioning maneuver | None | Epley for RPSC BPPV with improvement |
| 12 | F | 57 | Dizziness and instability. | DB nystagmus, maximum in DH to the right, with no response to ASC BPPV repositioning maneuver | None | Epley for LPSC BPPV with improvement | |
| 13 | F | 91 | Positional dizziness and instability. | DB nystagmus, maximum in DH to the left, with no response to ASC BPPV repositioning maneuver | None | Epley for RPSC BPPV with improvement | |
| 14 | M | 53 | Positional vertigo | DB nystagmus with no response to ASC BPPV repositioning maneuver; later on the patient develops positional nystagmus compatible with LPSC BPPV. | Normal | Epley for LPSC BPPV with symtoms resolution | |
| 15 | M | 70 | Positional vertigo | DB nystagmus with no response to ASC BPPV repositioning maneuver; later on the patient develops nystagmus compatible with RPSC BPPV. | Normal | Epley for RPSC BPPV with improvement | |
| 16 | F | 57 | Positional vertigo | DB nystagmus, maximum in DH to the left, with no response to ASC BPPV repositioning maneuver | Normal | Epley for RPSC with symptoms resolution | |
| 17 | F | 52 | Positional vertigo and instability. | DB nystagmus | None | Epley and Semont for RPSC BPPV with symptoms resolution | |
| 18 | F | 43 | LPSC BPPV | Positional vertigo and instability. | DB nystagmus | None | Epley for LPSC BPPV with symptoms resolution |
| 19 | F | 55 | Positional vertigo | DB nystagmus, maximum with DH to the right, with no response to ASC BPPV repositioning maneuver; later on the patient develops nystagmus compatible with LPSC BPPV. | Normal | Epley for LPSC with symptoms resolution | |
| 20 | M | 72 | RPSC BPPV | Instability | DB nystagmus with no response to ASC BPPV repositioning maneuver; later on the patient develops nystagmus compatible with RPSC BPPV. | Normal | Epley and Semont for RSC BPPV with symtoms improvement |
| Pat.: patient; BPPV: vértigo posicional paroxístico benigno; ACS: anterior semicircular canal; PCS: posterior semicircular canal; RPSC: right posterior semicircular canal; DB: downbeat; DH: Dix-Hallpike maneouver; LPSC: left posterior semicircular canal. | |||||||
| All the above patients were no responsive to ASC BPPV repositioning maneuvers | |||||||
Table 1:
Discussion
Recently the existence of ASC BPPV has been questioned and more specifically by the possible existence of apogeotropic PSC BPPV [4-6]. We have presented a series of patients who support this last point.
The explanation to justify the presence of downbeat nystagmus in BPPV of the posterior canal is that the otoconia would be in the non-ampullary distal arm of the posterior canal, near the common crus [3,4]
The Dix-Hallpike test, when the otoconias are close to the common crus, would cause the otoconia to move towards the dome, inhibiting the posterior channel, thus producing a downward vertical nystagmus with a torsional component of inhibitory type (Figure 1). This type of nystagmus could be triggered by both the Dix Hallpike maneuver (to the right or left), the Head-Hanging position, and even the lateral position. There is usually no latency, but it may have a crescendo-decrescendo course, and the nystagmus is not exhausted in the same way as the typical PSC BPPV. Rising to the upright position does not reverse the nystagmus direction, and it does not fatigue on repeated positional testing 3. This can be explained by arguing that the excitation of the anterior canal on one side produces the same type of nystagmus as the inhibition of the posterior canal on the other side [3-6]
One of the findings that is difficult to justify is the absence in a large proportion of patients of the torsional component, a phenomenon already described by Jacopo Campi., et al. [6] A plausible explanation, is that the vector of the torsional component is smaller than the one that comes from the posterior channel [6].
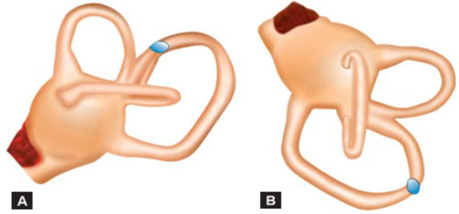
Figure 1A and B: Apogeotropic variant of PSC BPPV, the debris inside the PSC close to the common crus, gravitate toward the PSC ampullary arm.
Conclusion
While it cannot be stated that all BPPV with ASC compromise characteristics are an apogeotropic variant of PSC BPPV, the latter being more frequent than the previous one, it is expected that many positional down beating nystagmus are due to apogeotropic variant of the posterior semicircular canal. This last variant should be kept in mind when the patients did not respond to the typical replacement maneuvers for the ASC BPPV.
Conflict of interest
None.
None.
References
- Kim JS and Zee DS. “Clinical practice. Benign paroxismal positional vertigo”. otolaryngology-Head and Neck Surgery 370.12 (2014): 1138-1147.
- Von Brevern M., et al. “Benign paroxysmal positional vertigo: Diagnostic criteria”. Journal of Vestibular Research 25(2015): 105-117
- Welgampol MS., et al. “Neuro-otology- some recent clinical advances”. Journal of Neurology 264.1 (2017): 188-203
- Vannucchi P., et al. “Posterior Semicircular Canal Benign Paroxysmal Positional Vertigo Presenting with Torsional Downbeating Nystagmus: An Apogeotropic Variant”. International Journal of Otolaryngology (2012): doi:10.1155/2012/413603.
- Büki B. “Benign Paroxysmal Positional Vertigo - Toward New Definitions”. Otology and Neurotology 35.2 (2014): 323-328
- Cambi J., et al. “Natural course of positional down-beating nystagmus of peripheral origin”. Journal of Neurolology 260.6 (2013): 1489-1496.
Citation:
Sergio Carmona., et al. “Downbeating Nystagmus in Benign Paroxysmal Positional Vertigo: an Apogeotropic Variant of Posterior
Semicircular Canal”. Current Opinions in Neurological Science 1.6 (2017): 301-305.
Copyright: © 2017 Sergio Carmona., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.