Case Report
Volume 1 Issue 1 - 2017
A Report on Three Cases of NSTE-ACS on Optimal Medical Therapy with Surprising Atherosclerotic Plaque Regression
Department of Cardiology, Ruby General Hospital, Kolkata, India
*Corresponding Author: Anjan Dasgupta, Department of Cardiology, Ruby General Hospital, Kolkata, India.
Received: May 01, 2017; Published: May 27, 2017
Abstract
This paper presents three cases of male patients afflicted with Coronary Artery Disease (CAD). The patients presented at Emergency
Department (ED) with typical chest pain at rest. All of them were diagnosed to be suffering from Acute Coronary Syndrome
(ACS). Based on normal cardiac enzymes and ECG changes, the patients were classified into the category of Non-ST Elevation Acute
Coronary Syndrome (NSTE-ACS). All cases were hypertensive and dyslipidemic. After stabilisation, they underwent Coronary Angiography,
wherein Obstructive Coronary lesions, ranging from 80 to 95% mostly in the proximal Left Anterior Descending (LAD)
Artery, were detected. Guideline-based therapy demanded interventional strategies, namely Percutaneous Transluminal Coronary
Angioplasty (PTCA) or Coronary Artery Bypass Graft (CABG). But all the three patients opted for non-interventional treatment with
medicines only. The choice of therapy may be attributed to the total absence of symptoms with a combination of medications and lack
of financial affordability. These cases were treated in private hospitals where the cost was borne by the patients and their families.
In general, invasive procedure cost was 3 to 5 times that of conservative management [cost referred is in Indian context]. Selection
of these three cases was based out of author’s experience of treating nearly three hundred patients with Unstable Angina (UA) and
Non-ST-Elevation Myocardial Infarction (NSTEMI) [presently termed as NSTE-ACS] between 2001 and till date, in multiple centres,
primarily based on regular follow-up of over last sixteen years. The review Angiogram shows nearly complete plaque regression in
fifteen years and to 25-30% regression in just three years. As on date all of the three case-patients remain completely symptom-free
with regular normal activities only with Optimum Medical Therapy (OMT).
Keywords: Emergency Department (ED); Coronary Artery Disease (CAD); Optimal Medical Therapy (OMT); Acute Coronary Syndrome
(ACS); Non-ST Elevation Acute Coronary Syndrome (NSTE-ACS); Left Anterior Descending (LAD); Artery, Left Circumflex (LCX); Unstable
Angina (UA); Non-ST-Elevation Myocardial Infarction (NSTEMI)
Introduction
OMT is one of the recognised and approved modality of treatment of NSTE-ACS patients. This modality of treatment aims at patients overall well-being by preserving the quality of life with simple measures such as restrictions on undue exertions, limits on meal quantities, etc. Lifestyle changes are of enormous importance apart from medications in this form of treatment. Cessation of smoking, control of lipid anomalies, avoidance of weight gain and emphasis on Hypertension control are key issues. The general concept of “Short term ACS results are excellent but long term prognosis is significantly worse” [1]; this is the very fact that goes against two of my young patients referred here. The following case reports gave us a decade long experience of yielding some interesting longitudinal observations along with more light on this modality of treatment. The common thing in all these cases was that they all opted for medical management in spite of having an abnormal angiogram and having full awareness about the uncertain outcome with best of efforts. Although it has been clearly mentioned that “optimal medical management can be helpful in non-obstructive CAD, for obstructive CAD PCI with stenting should be preferred if available and affordable” [2], none of the patients in the cases referred here were motivated to go with the stenting option. Looking back, we can realise the tremendous benefits and positive results from choosing OMT form of treatment.
Case – 1
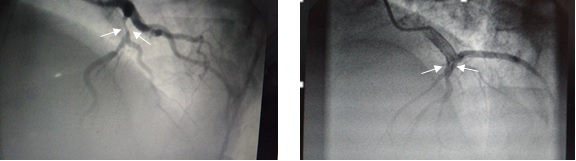
The Case 1 patient (48 year old male) was presented at ED with typical Chest pain in 2001 when he was only 32 years old. He had a history of Hypertension and was on medication for two years duration. The patient belonged to lower middle-class socioeconomic background (In Indian context middle class is defined as individuals with real annual household disposable income between $3080 and $15390). He had a normal BMI. He was a habitual smoker (five to ten cigarettes per day) but was a non-alcoholic. 12 lead ECG and Cardiac enzymes were normal when presented at ED and when taken 6 hours later. Lipid profile showed high LDLc, low HDLc, marginally raised TG and Lp(a) slightly above the normal value. His echocardiography showed hypokinetic anterior wall with preserved ejection fraction (LVEF). He was administered with standard treatment protocol for NSTE-ACS (previously termed UA) such as LMWH, ACEI (Perindopril), Beta Blocker (Metoprolol), IV NTG and oral Nitrates, dual Antiplatelets, Nicorandil, Ranolazine and full dose Statin (Atorvastatin). He was kept at CCU for 48 hours followed by dose titration outside CCU for another five days. With no recurrence of symptoms, he was subject to Coronary Angiogram with absolute care along with intracoronary Nitroglycerine (NTG 100 mcg at five min. interval). The angiogram revealed critical narrowing of LAD. After release from Hospital, he was on monthly check up for one year. Since then he visited the clinic after every two months for the 2nd year. From 3rd year onwards he used to report quarterly till review angiography was carried out in 2015 that showed complete disappearance (100%) of atheromatous plaque. HTN remained in well control throughout the entire duration of checkups. His LDLc always remained below 80 mg% (Target LDLc was 50-80 mg %). HDLc target was 40 mg%, but this remained in-between 35-40 on most examinations. The patient also maintained TG within normal range. Presently he is on twice a year follow up and continues to use Metoprolol, Perindopril and Atorvastatin at a maintenance dose. The patient can perform all normal activities with no symptoms. He never required a second hospitalisation since he was discharged sixteen years back related to the cardiac ailment. Shown below are the snapshots of angiograms taken in 2001 and 2015.
The Case 1 patient (48 year old male) was presented at ED with typical Chest pain in 2001 when he was only 32 years old. He had a history of Hypertension and was on medication for two years duration. The patient belonged to lower middle-class socioeconomic background (In Indian context middle class is defined as individuals with real annual household disposable income between $3080 and $15390). He had a normal BMI. He was a habitual smoker (five to ten cigarettes per day) but was a non-alcoholic. 12 lead ECG and Cardiac enzymes were normal when presented at ED and when taken 6 hours later. Lipid profile showed high LDLc, low HDLc, marginally raised TG and Lp(a) slightly above the normal value. His echocardiography showed hypokinetic anterior wall with preserved ejection fraction (LVEF). He was administered with standard treatment protocol for NSTE-ACS (previously termed UA) such as LMWH, ACEI (Perindopril), Beta Blocker (Metoprolol), IV NTG and oral Nitrates, dual Antiplatelets, Nicorandil, Ranolazine and full dose Statin (Atorvastatin). He was kept at CCU for 48 hours followed by dose titration outside CCU for another five days. With no recurrence of symptoms, he was subject to Coronary Angiogram with absolute care along with intracoronary Nitroglycerine (NTG 100 mcg at five min. interval). The angiogram revealed critical narrowing of LAD. After release from Hospital, he was on monthly check up for one year. Since then he visited the clinic after every two months for the 2nd year. From 3rd year onwards he used to report quarterly till review angiography was carried out in 2015 that showed complete disappearance (100%) of atheromatous plaque. HTN remained in well control throughout the entire duration of checkups. His LDLc always remained below 80 mg% (Target LDLc was 50-80 mg %). HDLc target was 40 mg%, but this remained in-between 35-40 on most examinations. The patient also maintained TG within normal range. Presently he is on twice a year follow up and continues to use Metoprolol, Perindopril and Atorvastatin at a maintenance dose. The patient can perform all normal activities with no symptoms. He never required a second hospitalisation since he was discharged sixteen years back related to the cardiac ailment. Shown below are the snapshots of angiograms taken in 2001 and 2015.
Case – 2
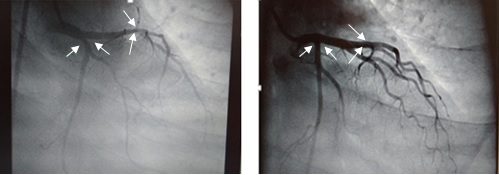
The case 2 patient (45 year old male) was admitted for severe chest pain in the year 2007 when the patient was just 35 years old. The symptoms were occurring for about two hours prior being admitted to the hospital, and the patient described the discomfort over the entire anterior chest. His ECG showed significant ST depression on Lead V1 to V4, but his cardiac enzymes were normal. Echo-doppler study showed hypokinesia of anterior wall (Antero-septal and Apical) with preserved ejection fraction (LVEF). His lipid profile revealed very low HDLc, mild to moderately raised LDLc, normal TG and very high Lp(a). The patient was from a middle-class socioeconomic background. The patient was a smoker (about ten cigarettes per day) but was a not an alcoholic. The patient was detected with mild to moderate Hypertension when admitted. He was found to be non-diabetic with normal BMI. Similar treatment regime initiated at CCU as per standard protocol mentioned in case-1. The patient responded very well with no recurrence of symptoms during the entire hospital stay. Coronary angiogram was abnormal with significant stenosis of proximal LAD and LCX. Both patient and his family disapproved to undergo PTCA. He remained on Optimal Medical Therapy, the same as described in the above case 1. Follow-up strategy was also the same. Review angiogram was conducted in 2015, and it showed that the coronary plaque regression came down to almost normal calibre arteries, from 80-90% occlusion in 2007. HTN remained well in control throughout the entire period of patient’s check-ups. His LDLc was maintained around 80 mg% while HDLc was just above 35 mg% on most occasions. There was complete cessation of smoking, and the BMI was maintained at a steady range of 20 to 25, average being 22. The patient never required another hospitalisation as far as coronary artery disease was concerned. Presently the patient is on Metoprolol (Extender Release), Clopidogrel, Rosuvastatin and is also physically very active with hobbies such as trekking and playing indoor sports.
The case 2 patient (45 year old male) was admitted for severe chest pain in the year 2007 when the patient was just 35 years old. The symptoms were occurring for about two hours prior being admitted to the hospital, and the patient described the discomfort over the entire anterior chest. His ECG showed significant ST depression on Lead V1 to V4, but his cardiac enzymes were normal. Echo-doppler study showed hypokinesia of anterior wall (Antero-septal and Apical) with preserved ejection fraction (LVEF). His lipid profile revealed very low HDLc, mild to moderately raised LDLc, normal TG and very high Lp(a). The patient was from a middle-class socioeconomic background. The patient was a smoker (about ten cigarettes per day) but was a not an alcoholic. The patient was detected with mild to moderate Hypertension when admitted. He was found to be non-diabetic with normal BMI. Similar treatment regime initiated at CCU as per standard protocol mentioned in case-1. The patient responded very well with no recurrence of symptoms during the entire hospital stay. Coronary angiogram was abnormal with significant stenosis of proximal LAD and LCX. Both patient and his family disapproved to undergo PTCA. He remained on Optimal Medical Therapy, the same as described in the above case 1. Follow-up strategy was also the same. Review angiogram was conducted in 2015, and it showed that the coronary plaque regression came down to almost normal calibre arteries, from 80-90% occlusion in 2007. HTN remained well in control throughout the entire period of patient’s check-ups. His LDLc was maintained around 80 mg% while HDLc was just above 35 mg% on most occasions. There was complete cessation of smoking, and the BMI was maintained at a steady range of 20 to 25, average being 22. The patient never required another hospitalisation as far as coronary artery disease was concerned. Presently the patient is on Metoprolol (Extender Release), Clopidogrel, Rosuvastatin and is also physically very active with hobbies such as trekking and playing indoor sports.
Case – 3
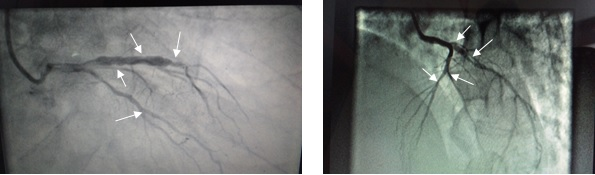
The case 3 patient (74 year old male) was admitted five years ago in 2012 at the age of 69 with typical chest pain through ED. His 12 lead ECG was abnormal, showing ST depression in Lead 1, avL, V1-V6. Cardiac Enzymes were normal. The patient had moderate Hypertension but did not have diabetes. Lipid profile was abnormal with low HDLc, high LDLc, moderately raised TG and raised Lp(a). His echo-doppler study revealed hypokinetic movement of the whole anterior wall with mildly reduced ejection fraction (LVEF 50%). The patient belonged to the upper-middle-class socioeconomic background and was a non-smoker with no addiction whatsoever. BMI was also within the normal range. This patient of NSTE-ACS was managed in line with the standard protocol of OMT, as already mentioned in Case 1. His angiogram showed significant coronary artery disease. He also declined to undergo PTCA without highlighting any particular reason. No amount of persuasion could motivate him to undergo PTCA. This patient too showed a promising result with medications only, remaining completely symptom-free during the entire hospital stay of 7 to 8 days. He had no recurrence of chest pain till date. Review angiogram in 2015 showed regression of plaque to a very satisfactory level in just three years. His present medications include Metoprolol, Nitrates, Perindopril, clopidogrel, Ranolazine and Atorvastatin. In spite of his plaque regression, his medications remain same as on date, due to his effortful walking as a result of Osteoarthritis in Knee joints. This patient also did not require any further hospitalisation on Cardiac reason. HTN remained well control all throughout the patient’s check-up period. Over the period of treatment, the lipid profile of the patient improved. LDLc was below 80 mg % while HDLc was just above 35 mg% on most occasions. His TG also remained at the upper normal value.
The case 3 patient (74 year old male) was admitted five years ago in 2012 at the age of 69 with typical chest pain through ED. His 12 lead ECG was abnormal, showing ST depression in Lead 1, avL, V1-V6. Cardiac Enzymes were normal. The patient had moderate Hypertension but did not have diabetes. Lipid profile was abnormal with low HDLc, high LDLc, moderately raised TG and raised Lp(a). His echo-doppler study revealed hypokinetic movement of the whole anterior wall with mildly reduced ejection fraction (LVEF 50%). The patient belonged to the upper-middle-class socioeconomic background and was a non-smoker with no addiction whatsoever. BMI was also within the normal range. This patient of NSTE-ACS was managed in line with the standard protocol of OMT, as already mentioned in Case 1. His angiogram showed significant coronary artery disease. He also declined to undergo PTCA without highlighting any particular reason. No amount of persuasion could motivate him to undergo PTCA. This patient too showed a promising result with medications only, remaining completely symptom-free during the entire hospital stay of 7 to 8 days. He had no recurrence of chest pain till date. Review angiogram in 2015 showed regression of plaque to a very satisfactory level in just three years. His present medications include Metoprolol, Nitrates, Perindopril, clopidogrel, Ranolazine and Atorvastatin. In spite of his plaque regression, his medications remain same as on date, due to his effortful walking as a result of Osteoarthritis in Knee joints. This patient also did not require any further hospitalisation on Cardiac reason. HTN remained well control all throughout the patient’s check-up period. Over the period of treatment, the lipid profile of the patient improved. LDLc was below 80 mg % while HDLc was just above 35 mg% on most occasions. His TG also remained at the upper normal value.
Discussion
The principal objective of highlighting these three cases is as follows: These patients had some important features in common. All of them belonged to the similar socioeconomic background (middle-class) and had Hypertension along with Dyslipidemia. Two of them were regular smokers at the time of the Coronary event, and they developed the disease at age, below 35 years. A Longitudinal observation in the younger age group patients did very well contrary to the general belief and reports [1].
This case reports are sharply in contrast to the statement of “the increase in disease and availability of facilities has resulted in a dramatic change, and the focus is shifting from only medical treatment to invasive treatment” [3]. The two young patients were not in the category of sedentary lifestyle, which was found to be the major modifiable risk factor for IHD by Zahidullah M., et al. Also, they had hypertension and dyslipidemia, those being the second most important modifiable risk factor [4]. From the given cases it can be observed beyond doubt that tight control of modifiable risk factors is the key issues in the long term benefit of CAD, whether in young or elderly patients.
Conclusion
All three cases were ideal candidates for interventional strategies such as PTCA or CABG as per existing guidelines. None of the patients could be motivated for any interventional strategies for reasons best known to them. All remained asymptomatic with just OMT. These patients, referred in the study were ideal patients in terms of changing their lifestyles (by quitting Smoking), taking regular medicines, having a healthy diet, performing graded exercise and also conducting periodical follow-ups. As far as Statins are considered, these drugs do cause atheromatous plaque stabilisation and regression. It remains to be extrapolated that whether Statins alone made so much of reduction of plaque burden or ACEI also contributed to this effect. It was surprising that a critically narrowed LAD would become a nearly normal calibre vessel in fifteen years or so with OMT and lifestyle modification. At the same time, significant plaque regression in just three years was also very encouraging that any patient who is unwilling for interventional therapies may well opt for Medical Therapy alone. It seems that the key reasons for opting Optimal Medical Therapy (OMT) are a lack of cathlab facility at the hour of need, financial unaffordability and lack of motivation.
This conservative management needs to be revisited not only based on these three case reports but also based on further research. There is a definite need to investigate such an enormous atheromatous plaque regression, especially in countries where the cost of treatment is borne almost entirely by the patient, and the states’ contribution is insignificant.
References
- Maroszyńska-Dmoch EM and Wożakowska-Kapłon B. “Clinical and angiographic characteristics of coronary artery disease in young adults: a single centre study”. Kardiologia Polska74.4 (2016): 314-321.
- Jamshed Dalal., et al. “Vascular Disease in Young Indians (20-40 years): Role of Ischemic Heart Disease”. Journal of Clinical and Diagnostic Research 10.9 (2016): OE08–OE12.
- Association of Physicians of India. “API expert consensus document on management of Ischemic heart disease”. The Journal of the Association of Physicians of India54 (200): 469-480.
- Zahidullah M., et al. “Evaluation of Patients with Coronary Artery Disease for major modifiable risk factors for Ischemic Heart Disease”. Journal of Ayub Medical College Abbottabad 24.2 (2012): 102-105.
Citation:
Anjan Dasgupta. “A Report on Three Cases of NSTE-ACS on Optimal Medical Therapy with Surprising Atherosclerotic Plaque
Regression”. Therapeutic Advances in Cardiology 1.1 (2017): 31-35.
Copyright: © 2017 Anjan Dasgupta. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.





























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.