Research Article
Volume 2 Issue 2 - 2018
Retinoblastoma in Mongolia: Clinical Characteristics and Survival from 1987 to 2017
1Department of Ophthalmology, National Center for Maternal and Child Health, Mongolia
2Department of Ophthalmology, Mongolian National University of Medical Sciences
2Department of Ophthalmology, Mongolian National University of Medical Sciences
*Corresponding Author: Tsengelmaa Chuluunbat, Department of Ophthalmology, National Center for Maternal and Child Health, 16060 Khuvisglachdiin Street, Bayangol district, Ulaanbaatar, Mongolia.
Received: April 09, 2018; Published: June 02, 2018
Abstract
Purpose: To describe the clinical characteristics and the treatment outcome of retinoblastoma in Mongolian children.
Methods: Data of all children diagnosed with retinoblastoma at the National Center for Maternal and Child Health of Mongolia from 1987 to January 2017 were reviewed retrospectively and prospectively. The information on laterality of tumor, clinical presentations, immunohistiochemical analysis and mode of treatment were obtained. Survival characteristics of the cohort were analyzed.
Results: Retinoblastoma was diagnosed in 100 eyes of 79 cases during the study period. Median age of diagnosis was 23.2 ± 5.8 months. There were no differences in sex ratio and 21 cases (27%) were bilateral. Fifty-two patients (66%) were from rural areas. The more frequent clinical presentations were leukocoria in 64 (81%) patients, strabismus in 34 (44 %) patients and unilateral mydriasis in 35 (45%) patients. Sixty-nine patients (87.3%) were diagnosed of Classification D or worse when presented to us. Due to late diagnosis in the majority of cases, unilateral and bilateral enucleations were performed in 58 (58%) cases and 26 (26%) eyes respectively; exenteration was done in 3 cases (3%), intravenous chemotherapy was done (11%) eyes and laser surgery was done (4%) eyes. At the time of last follow-up, 72 (93.1%) patients were alive, five (6.3%) patients were dead, and seven (9%) patients had lost to follow-up or unknown vital status. The mean follow-up period was 144.1 ± 16.3 (95% CI 122.6-165.5) months (range, 15-365 months). In five cases with immunohistochemistry analysis in the eye specimen, neuronspecific enolase-, Ki-67 protein-, and B-cell lymphoma 2-positive cells were found in all five (100%) cases and Rb protein was detected in three (60%) cases.
Conclusion: The implementation of International classification of RB, systemic intravenous chemotherapy and laser treatment for retinoblastoma, shows favorable outcome in the treatment of RB and further prognosis.
Introduction
Retinoblastoma is the most common intraocular malignant tumor in childhood and it is a serious ocular malignancy that manifests covertly with painless leukocoria and threatens survival of the patient [1,2].
The primary strategy for retinoblastoma management is focused on patient survival, and the secondary goals are to salvage the globe and vision of the patients [3-5].
The survival of the children is markedly dependent on an early diagnosis shortly after the detection of symptoms such as leukocoria or squinting. The delay in the clinical diagnosis may depend on the medical infrastructure of the country and on the alertness of the parents as well as of the pediatricians [6].
Mongolia is the big country with sparsely population. It is a developing country without updated medical equipment and facility. Only three to four new cases of retinoblastoma each year are estimated in Mongolia. However, retinoblastoma is an emerging health issue with problems of late diagnosis and poor visual outcome in Mongolia [7].
Prior studies of retinoblastoma were reported only in Mongolian and had gained little international attention [7]. In this paper, we aim to update the profiles and outcome of retinoblastoma from the leading National Center for Maternal and Child Health in Mongolia.
Materials and Methods
Data of all children diagnosed with retinoblastoma from 1987 to 2017 at the National Center for Maternal and Child Health of Mongolia were reviewed retrospectively with approval from the Institutional Review Board of Mongolian National University of Medical Science. The ICRB classification was used. Survival characteristics of the cohort were analyzed.
The data recorded included jurisdiction, sex, date of birth, age at diagnosis, and information on laterality of tumor, family history of retinoblastoma, clinical presentations and mode of treatment. The diagnosis of retinoblastoma was based on the results of slit lamp examination, indirect ophthalmoscope, echography, computerized tomography, or magnetic resonance imaging depending on the availability of the tools. In treatment, laser surgery, enucleation and exenteration combined with systemic chemotherapy were used for these patients.
Survival time of the cohort were documented and analyzed.
Histologic Assessment and Immunohistochemical Assessment
With hematoxylin and eosin stain, the extent of tumor in optic nerve, choroid and anterior chamber were scored and confirmed by pathologists. The immunohistochemistry of RB was performed at Beijing Tongren Hospital, China. The expressed protein checked in this study included retinoblastoma protein, neuron-specific enolase, s-100 protein, p53, vimentin, bcl-2, ki67 and glial fibrillary acidic protein.
With hematoxylin and eosin stain, the extent of tumor in optic nerve, choroid and anterior chamber were scored and confirmed by pathologists. The immunohistochemistry of RB was performed at Beijing Tongren Hospital, China. The expressed protein checked in this study included retinoblastoma protein, neuron-specific enolase, s-100 protein, p53, vimentin, bcl-2, ki67 and glial fibrillary acidic protein.
Statistical Analysis
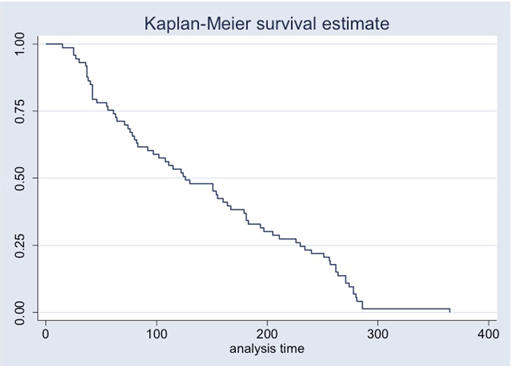
The data of retinoblastoma patients at our center from1987 to 2017 were collected and analyzed. The data were presented as descriptive statistics. Patient survival were calculated and analyzed using the Kaplan-Meier method. Data were expressed as mean ± SD.
The data of retinoblastoma patients at our center from1987 to 2017 were collected and analyzed. The data were presented as descriptive statistics. Patient survival were calculated and analyzed using the Kaplan-Meier method. Data were expressed as mean ± SD.
Results
Patients
One hundred eyes of 79 children were diagnosed of Retinoblastoma at the Department of Ophthalmology, National Center for Maternal and Child Health of Mongolia from January 1987 to March 2017. Our hospital is the only hospital that treats and takes care of retinoblastoma patients in Mongolia, it was therefore estimated the incidence of retinoblastoma was about 1 to 23,000-24,000 live births. Among these 79 patients, 52 patients (66%) were from rural areas and 27 patients (34%) were from urban area.
One hundred eyes of 79 children were diagnosed of Retinoblastoma at the Department of Ophthalmology, National Center for Maternal and Child Health of Mongolia from January 1987 to March 2017. Our hospital is the only hospital that treats and takes care of retinoblastoma patients in Mongolia, it was therefore estimated the incidence of retinoblastoma was about 1 to 23,000-24,000 live births. Among these 79 patients, 52 patients (66%) were from rural areas and 27 patients (34%) were from urban area.
Sex and Laterality
There was equal distribution in sex ratio in our patients. Among the patients, 39 (49.4%) were boys and 40 (50.6%) were girls. In location, it was unilateral in 58 (73.4%) patients and bilateral in 21 (27%) patients. The disease was familial in two patient (2.5%) and sporadic in 77 (97.5%) (Table1).
There was equal distribution in sex ratio in our patients. Among the patients, 39 (49.4%) were boys and 40 (50.6%) were girls. In location, it was unilateral in 58 (73.4%) patients and bilateral in 21 (27%) patients. The disease was familial in two patient (2.5%) and sporadic in 77 (97.5%) (Table1).
| No. of Cases | % | |
| Sex | ||
| Male | 39 | 49.4 |
| Female | 40 | 50.6 |
| Laterality | ||
| Unilateral | 58 | 73.4 |
| Bilateral | 21 | 27 |
| Family history | ||
| Yes | 2 | 2.5 |
| No | 77 | 97.5 |
Table 1: Characteristics of Patients with Retinoblastoma (1987-to January 2017, Mongolia).
Age at Diagnosis
Age of diagnosis ranged from 1-72 months. Mean age of diagnosis was 23.2 ± 5.8 months. Fifty-three (86,1%) patients were diagnosed before the age of 3. The age at diagnosis was lower in bilateral cases (mean age 13.9 ± 2.4, months range 1-42) than in unilateral cases (mean age 26.6 ± 1 months, range 1-72).
Age of diagnosis ranged from 1-72 months. Mean age of diagnosis was 23.2 ± 5.8 months. Fifty-three (86,1%) patients were diagnosed before the age of 3. The age at diagnosis was lower in bilateral cases (mean age 13.9 ± 2.4, months range 1-42) than in unilateral cases (mean age 26.6 ± 1 months, range 1-72).
Presenting Signs
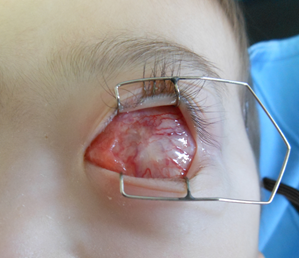
The most prevalent clinical conditions were leukocoria in 64 patients (81%), strabismus in 34 patients (43%), unilateral mydriasis in 35 patients (44.3%), glaucoma in 26 patients (33%), hyphema in 9 patients (11%) patients and orbital cellulitis in 5 patients (6.3%) respectively. Three patients (4.7%) presented as late-stage, extraocular stage of RB (Figure 1).
The most prevalent clinical conditions were leukocoria in 64 patients (81%), strabismus in 34 patients (43%), unilateral mydriasis in 35 patients (44.3%), glaucoma in 26 patients (33%), hyphema in 9 patients (11%) patients and orbital cellulitis in 5 patients (6.3%) respectively. Three patients (4.7%) presented as late-stage, extraocular stage of RB (Figure 1).
Disease Detection
Since there were no eye screening program in Mongolia, all patients (100%) were referring to ophthalmologists for further evaluation due to various presenting signs mentioned above. 54 (68.3%) patients was examined with B scan, 52 (66%) patients with CT and 45 (56%) patients with MRI, 15 (19%) patients was examined with Retcam respectively.
Since there were no eye screening program in Mongolia, all patients (100%) were referring to ophthalmologists for further evaluation due to various presenting signs mentioned above. 54 (68.3%) patients was examined with B scan, 52 (66%) patients with CT and 45 (56%) patients with MRI, 15 (19%) patients was examined with Retcam respectively.
Spread of Tumor
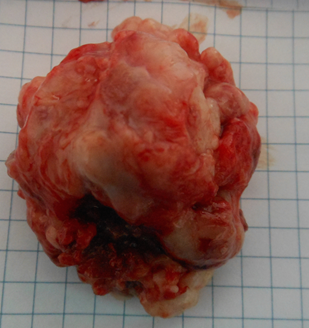
One case (1.2%) with intracranial extension, three cases (3.8%) had extra ocular extension and one case (1.2%) developed the orbital recurrence of retinoblastoma four years after initial enucleation (Figure 2 and 3). The other 74 patients (93.6 %) had intraocular retinoblastoma without any extraocular extension.
One case (1.2%) with intracranial extension, three cases (3.8%) had extra ocular extension and one case (1.2%) developed the orbital recurrence of retinoblastoma four years after initial enucleation (Figure 2 and 3). The other 74 patients (93.6 %) had intraocular retinoblastoma without any extraocular extension.
Figure 2: Orbital recurrence of retinoblastoma, four years
after the initial enucleation, left eye in a 5 years old girl.
Figure 3: The exenteration specimen measured 47 x 53 x 39 mm. A large tumor invaded
the connective tissue and muscle, and extended to the superior surgical margin not completely
resected. Histopathological examination disclosed an undifferentiated recurrent
retinoblastoma. The patient died 5 months after the exenteration.
Mode of Treatment
Enucleation in one eye was performed in 58 eyes (58 %), bilateral enucleation in 26 eyes (26 %) and exenteration in 3 eyes (3%) in the early years of this study. Additional exenteration was done one eye due to orbital of recurrence retinoblastoma after four years of initial enuleation. Four eyes (3%) received the local laser treatment and eleven (11%) eyes received systemic intravenous chemotherapy only and the tumors were stable with partial regression (Table 2).
Enucleation in one eye was performed in 58 eyes (58 %), bilateral enucleation in 26 eyes (26 %) and exenteration in 3 eyes (3%) in the early years of this study. Additional exenteration was done one eye due to orbital of recurrence retinoblastoma after four years of initial enuleation. Four eyes (3%) received the local laser treatment and eleven (11%) eyes received systemic intravenous chemotherapy only and the tumors were stable with partial regression (Table 2).
| No of Eyes | % | |
| Unilateral enucleation | 58 | 58 |
| Bilateral enucleation | 26 | 26 |
| Unilateral exenteration | 3 | 3 |
| Laser photocoagulation therapy with Systemic intravenous chemotherapy | 2 | 2 |
| Systemic intravenous chemotherapy | 9 | 9 |
| Laser treatment | 2 | 2 |
Table 2: Mode of treatment in Retinoblastoma cases.
Histology
Eighty-seven eyeballs were subjected for histopathological examination after enucleation, Histologically undifferentiated type was in 46 eyes (53%), optic nerve infiltration was in 5 eyes (5.7 %), Rosettes was in 5 eyes (5.7%), calcification 4 eyes (4.5%), hemorrhage was in 2 eyes (2.3%) and necrosis was in one eye (1.1%) respectively (Table 3). Rest of them 24 eyes (27.6%) was unclear due to not written on the patient’s chart.
Eighty-seven eyeballs were subjected for histopathological examination after enucleation, Histologically undifferentiated type was in 46 eyes (53%), optic nerve infiltration was in 5 eyes (5.7 %), Rosettes was in 5 eyes (5.7%), calcification 4 eyes (4.5%), hemorrhage was in 2 eyes (2.3%) and necrosis was in one eye (1.1%) respectively (Table 3). Rest of them 24 eyes (27.6%) was unclear due to not written on the patient’s chart.
| Histological findings | Number (%) |
| Undifferentiated type | 46 (53%) |
| Optic nerve infiltration | 5 (5.7%) |
| Rosettes | 5 (5.7%) |
| Calcification | 4(4.5%) |
| Necrosis | 1(1.1%) |
| Haemorrhage | 2(2.3%) |
Table 3: Histopathological findings in retinoblastoma (n = 87 eyes).
Immunochemistry analysis.
Enucleated eyes of 5 children were used for histology and Immunochemistry analysis study. Histologically, four tumors (80%) were classified as undifferentiated retinoblastoma and one case (20%) was differentiated retinoblastoma on the basis of the presence of areas containing Flexner-Wintersteiner rosettes and fleurettes (Table 4). In 5 cases with immunohistochemistry analysis in the eye specimen, neuron-specific enolase (NSE), Ki-67 protein (Ki-67), B-cell lymphoma 2 (Bcl-2) positive cells were found in all of 5 (100%) cases and Rb protein was detected in 3(60%) cases. Pathologically, two in 5 cases (40%) demonstrated nerve involvement, three cases (60%) with RPE involvement, two cases (40%) choroid involvement, two cases (40%) had a calcification. The detailed information of the immunohistochemistry is shown in Table 4.
Enucleated eyes of 5 children were used for histology and Immunochemistry analysis study. Histologically, four tumors (80%) were classified as undifferentiated retinoblastoma and one case (20%) was differentiated retinoblastoma on the basis of the presence of areas containing Flexner-Wintersteiner rosettes and fleurettes (Table 4). In 5 cases with immunohistochemistry analysis in the eye specimen, neuron-specific enolase (NSE), Ki-67 protein (Ki-67), B-cell lymphoma 2 (Bcl-2) positive cells were found in all of 5 (100%) cases and Rb protein was detected in 3(60%) cases. Pathologically, two in 5 cases (40%) demonstrated nerve involvement, three cases (60%) with RPE involvement, two cases (40%) choroid involvement, two cases (40%) had a calcification. The detailed information of the immunohistochemistry is shown in Table 4.
| Case/ID | Case1/0033 | Case2/0034 | Case3/0037 | Case4/0042 | Case5/0053 |
| Code | X-1279 | X-797 | X-171 | X-27 | X-1345 |
| Pathological type | Undifferentiated | Undifferentiated | Differentiated | Undifferentiated | Undifferentiated |
| Nerve involvement | NA | + | - | + | NA |
| RPE involvement | + | + | - | + | - |
| Choroid involvement | + | + | - | NA | - |
| Calcification | - | + | NA | - | + |
| Immunohistochemistry | |||||
| RB | + | + | - | + | + |
| Bcl-2 | + | + | + | + | + |
| Ki-67 | + | + | + | + | + |
| NSE | + | + | + | + | + |
| Vimentin | -/Stromal cells (+) | + | -/Stromal cells (+) | + | + |
| GFAP | + | + | -/Stromal cells (+) | - | + |
| P-53 | + | - | + | - | + |
| S100 | + | + | - | NA | + |
Table 4: Histopathologic and Immunohistochemical result of five patients who has been done enucleation.
RPE = retinal pigment epithelium; Rb = Retinoblastoma protein; Bcl-2 = B-cell lymphoma 2; Ki-67 = protein that in humans is encoded by the MKI67 gene (antigen identified by monoclonal antibody Ki-67); NSE = neuron-specific enolase; Vimentin = An immunohistochemical study of vimentin; GFAP = glial fibrillary acidic protein; P-53 = Tumor protein p53; S-100 = low-molecular-weight protein
RPE = retinal pigment epithelium; Rb = Retinoblastoma protein; Bcl-2 = B-cell lymphoma 2; Ki-67 = protein that in humans is encoded by the MKI67 gene (antigen identified by monoclonal antibody Ki-67); NSE = neuron-specific enolase; Vimentin = An immunohistochemical study of vimentin; GFAP = glial fibrillary acidic protein; P-53 = Tumor protein p53; S-100 = low-molecular-weight protein
Follow
At time of last follow-up, 67 patients (85%) were alive, 5 patients (6.3%) were dead and 7 patients (8.8%) had unknown vital status. The mean follow-up was 144.1 ± 16.1 months. Median survival time was 144.1 months (Figure 4). The longest follow-up was 32 years in a male with bilateral retinoblastoma, and his son was born with inherited bilateral retinoblastoma. Enucleation of father’s right eye and left eye was done at the age of 3 months and 44 months respectively. His son also received with bilateral enucleation at the age of 2 months in right eye, and at the age of 61 months in left eye. Four patients (6%) died due to delayed diagnosis of retinoblastoma with the presentation of extra ocular extension and intracranial spread.
At time of last follow-up, 67 patients (85%) were alive, 5 patients (6.3%) were dead and 7 patients (8.8%) had unknown vital status. The mean follow-up was 144.1 ± 16.1 months. Median survival time was 144.1 months (Figure 4). The longest follow-up was 32 years in a male with bilateral retinoblastoma, and his son was born with inherited bilateral retinoblastoma. Enucleation of father’s right eye and left eye was done at the age of 3 months and 44 months respectively. His son also received with bilateral enucleation at the age of 2 months in right eye, and at the age of 61 months in left eye. Four patients (6%) died due to delayed diagnosis of retinoblastoma with the presentation of extra ocular extension and intracranial spread.
| Author | Year | Country | No. of patients | Leukocoria | Strabismus | Proptosis |
| Abramson., et al. [12] | 1998 | USA | 1265 | 56.1 | 23.6 | 0.5 |
| Tarkkanen & Tuoveinen [23] |
1971 | Finland | 136 | 39.7 | 13.2 | - |
| Bedford., et al. [24] | 1971 | UK | 139 | 23.2 | 14.2 | - |
| Tan., et al. [25] | 1997 | Singapore | 41 | 82.9 | 19.5 | - |
| Chantada., et al. [26] | 1999 | Argentina | 95 | 81 | 14.3 | - |
| Peterson [16] | 2000 | USA | 114 | 61.4 | 18.4 | - |
| Patikulsila & Patikulsila [27] | 2001 | Thailand | 30 | 60 | 10.0 | 26.7 |
| Kao., et al. [28] | 2002 | Taiwan | 96 | 78.1 | 12.5 | 16.7 |
| Dondey., et al. [29] | 2004 | Australia | 165 | 53.3 | 26.0 | - |
| Shanmugam., et al. [30] | 2005 | India | 355 | 74.6 | 6.2 | 1.1 |
| Badhu., et al. [15] | 2005 | Nepal | 43 | 32.5 | - | 44.2 |
| Ozkan., et al. [8] | 2006 | Turkey | 141 | 82.2 | 9.2 | 7.8 |
| Chung., et al. [31] | 2008 | South Korea | 70.0 | 80.0 | 8.5 | 1.4 |
| Rai., et al. [14] | 2009 | Pakistan | 53 | 22.6 | 5.6 | 52.8 |
| Bonanomi., et al. [33] | 2009 | Brazil | 28 | 75.0 | 10.7 | 3.6 |
| Naseripour., et al. [34] | 2009 | Iran | 105 | 64.8 | 28.2 | - |
| Reddy at all [35] | 2009 | Malaysia | 64 | 71.8 | 9.3 | 32.8 |
| Present study | 2017 | Mongolia | 79 | 81 | 43 | 4.6 |
Table 5: Comparative frequency of common presenting signs of retinoblastoma in different parts of World.
Discussion
In the worldwide studies retinoblastoma has no sex ratio difference, and the average age at diagnosis is 18 months and the vast majority become clinically apparent before the age of 3 years. In most of the developed countries patients with bilateral tumors present earlier than those with unilateral involvement [1,4]. In our studies also, there was not much difference in the sex of retinoblastoma in boys (49.4%) and girls (50.6%). The mean age of patients at presentation was 23.2 months and 86.1% were below 36 months age. The mean diagnosed age was less in bilateral cases (13.9 months) than in unilateral cases (26. M6onths). The age at initial diagnosis is 25 months in Brazil, 25 months in Turkey and 18 months in America [8-10] 23.2 months in Mongolia.
Leukocoria is the most common presenting sign of retinoblastoma followed by strabismus all over the world (Table 5). The figures vary from country to country, from time to time in the same country. This could probably be due to geographical variation of the disease, awareness of the disease among the public, availability of medical facilities in that country and number of patients examined. The frequency of common modes of presentation in our study is consistent with many studies different from parts of the world. In our study series, initial disease detection were leukocoria, strabismus, and therefore poor ocular survival rates for the presenting eye. In our analysis of 100 eyes with retinoblastoma, globe salvage and preserve vision was 13 eyes (13%), lower than for developed country’s patients. As for the survival, 67 patients (85%) were survival, 7 patients (8.8%) had unknown vital status and 5 patients (6.3%) died.
The average incidence of retinoblastoma varies by race or geographic location, but the average incidence is approximately one in 15 000 newborns [8, 11-13]. In Mongolia the average incidence estimates about one in 23,000-24,000 live birth [7] . Although the age at initial diagnosis varies, early detection is important to achieve better treatment results.
Initial disease detection at the point of leukocoria or strabismus usually correlated with high in patient survival rates but poor ocular survival rates for the presenting eye in the past, when chemoreduction and SOAI were not instituted as a regular treatment.
Saving eyes and vision requires disease recognition before leukocoria, as demonstrated by the better ocular salvage rate among patients who had a positive family history and received clinical surveillance via early, routine dilated funduscopic examinations by an ophthalmologist [10].
In addition to the above, Abramson., et al. [10] reported many uncommon/rare presenting signs viz anisocoria, heterochromia iridis, inflammatory signs, nystagmus, microphthalmia/buphthalmos, proptosis, orbital cellulitis, hyphema, ptosis,
haemorrhage
retinoblastoma.
However, proptosis as the presenting sign at the time of diagnosis was reported in high frequency from some of the developing countries like Nigeria (84.6%) [12], Pakistan (52.8%) [14], Nepal (44.2%) [15], Thailand (26.7%) [16] and India (25.3%)[17]. In our studies, presenting signs of leukocoria, strabismus and secondary glaucoma were seen in 78%, 38%, and 33% of our patients. Bilateral retinoblastoma was seen in 26.5% of patients in our case series which was lower to the figures reported from USA (41.5% ) [10], Australia (41% ) [18], India (37.2% ) [17], and Thailand (36.7%) [16].
Early diagnosis and prompt treatment are important factors in achieving high survival rates. In developing countries, late referral has been implicated as been established yet [19] .
Chemotherapy has achieved an important role in the management of intraocular retinoblastoma. We have used the standard intravenous chemotherapy (etopside, carboplatin, vincristine) for intraocular retinoblastoma since 2012 in Mongolia, even though enucleation is still done frequently in advanced cases including large tumors, neovascular glaucoma, pars plana tumor seeding, anterior chamber involvement or choroid, optic nerve or orbital tumor extension, with no expectation for useful vision.
External beam radiotherapy, although effective, can result in cosmetic deformity, cataracts, or retinopathy and carries an increased risk of a second non-ocular malignancy in the treatment field [34]. Focal therapies such as cryotherapy, laser and plaque radiotherapy have been used to treat eyes with RE group 1 to 3 tumors to avoid enucleation and EBRT and small tumors with no evidence of seeding. A combination of focal therapy with chemoreduction has provided an alternative to the treatment of large tumors with primary enucleation [20]. Chemoreduction utilizes neoadjunctive chemotherapy to reduce the tumor volume and enable focal therapy [3,10].
Worldwide, the incidence of retinoblastoma is recorded to be about 11 cases per million children younger than 5 years. A more commonly used estimate is 1 case of retinoblastoma per 18,000-30,000 live births, depending on the country.
An estimated 250-500 new cases of retinoblastoma occur in the United States yearly. In the Philippines, unpublished reports have estimated the incidence to be more than 1 case of retinoblastoma per 18,000 live births.
Over half of Mongolia’s population of 3 million people dwell in the capital of Ulaanbaatar, but the remaining 45%, nearly half of whom are nomads, are thinly spread over what is the world’s 19th largest country by land mass. While Ulaanbaatar has over 100 ophthalmologists at nearly a dozen small and large public and private hospitals, access to high-quality pediatric eye care services is very limited in rural areas.
Of all 20,496 patients admitted to the Ophthalmology Department between January 1987 and January 2014. It is estimated about 1 to 32,000-33,000 live births [7]. We are the only children hospital in Mongolia to receive and treatment RB patients.
Established in 1987, NCMCH is the country’s center of excellence for pediatric and maternal health care. The ophthalmology department provides eye care to children from all over the country. NCMCH is the sole training hospital for residents in pediatric ophthalmology in Mongolia. However the ophthalmology department has little functional equipment and a comprehensive framework to treat children’s eye disease is lacking in Mongolia including a radiologist, pediatric oncologist, ophthalmic oncologist and medical facility.
Delaying diagnose, loosing follow up of retinoblastoma are leading cause of the late potential outcome in children. In our analysis of 100 eyes with retinoblastoma, globe salvage and preserve vision was 13 eyes (13%), lower than for developed country’s patients. As for the survival, 67 patients (85%) were survival, 7 patients (8.8%) had unknown vital status and 5 patients (6.3%) were died.
The retinoblastoma (Rb) protein is a tumor suppressor protein that is inactivated and results in development of retinoblastoma cancer. In our series, three in 5 cases (60%) were detected to express Rb protein on immunochemistry analysis.
Neuron-specific enolase (NSE) is a substance that has been detected in patients with certain tumors and stained strongly positive in undifferentiated tumor cells and weakly positive in rosettes and fleurettes in most of the cases (21/27) [21]. In our study, NSE positive cells were found in all of 5 retinoblastoma cases and 80% of them were classified the undifferentiated retinoblastoma cell. Bcl-2 (B-cell lymphoma 2) is the founding member of the Bcl-2 family of apoptosis regulator proteins encoded by the BCL2 gene. Some authors explained that expression of Bcl-2 was significantly higher in the invasive tumour tissues (P = 0.0001) as compared with the non-invasive tumours by immunohistochemistry.
Glial fibrillary acidic protein (GFAP) is an intermediate filament (IF) protein that was thought to be specific for astrocytes in the central nervous system (CNS). The Ki-67 protein (also known as MKI67) is a cellular marker for proliferation. It is strictly associated with cell proliferation.
Neuron-specific enolase (NSE), The Ki-67 protein (Ki-67), B-cell lymphoma 2 (Bcl-2) positive cells were found in all of 5 retinoblastoma (100%) cases respectively in our study.
Immunocytochemistry of paraffin-embedded tissues of the neoplasms revealed immunoreactivity with antibodies against S-100 protein, glial fibrillary acidic protein (GFAP), vimentin, neuron-specific enolase(NSE) and bcl-2. S-100, GFAP and vimentin were positive only for glial elements (reactive astrocytes) and, NSE and bcl-2 for almost all tumor cells. These findings support the previous reports that the majority of retinoblastomas are sporadic. The results of this study also support the views that retinoblastomas are composed of neuron-committed cells [22].
In the normal retina, S-100 protein, glial fibrillary acidic protein (GFAP) and vimentin were detected in astrocytes and/or Müller cells. Neurofilament protein was seen in axons of the ganglion cells, synaptophysin was present in both plexiform layers, bcl-2 oncoprotein was seen in ganglion cells and bipolar cells, and neuron-specific enolase (NSE) was detected in ganglion cells, bipolar cells and photoreceptor cells and in their cell processes [23]. Most rosettes and fleurettes, and some undifferentiated cells in retinoblastomas were NSE positive, GFAP and S-100 positive cells in retinoblastomas were detected mostly in well differentiated glial cells. It means that retinoblstoma may arise from primitive bipotential or multipotential cells capable of neuronal and glial differentiation [24]. Other proteins of 5 cases weren’t analyzed completely on immunochemistry analysis due to some poor tissue quality. However, Vimentin was detected in two cases, Stromal cells expressed vimentin on two cases, glial fibrillary acidic protein (GFAP) on three cases, P-53 on two cases, and S-100 on three cases in our study.
In our series, we found that undifferentiated type 46 eyes (53%) were the most common type of histological finding for advanced retinoblastoma in Mongolian patients. Kashyap., et al. identified poorly differentiated retinoblastoma presented in 80.3% and well-differentiated in 19.7% of 609 enucleated eyes for advanced intraocular retinoblastoma. Well- differentiated tumors presented earlier (median 1.2 years) than poorly differentiated tumors (median 2.5 years) (p < .001) [25].
The limitation of this study series, some of the patients diagnosis was not classified the international intraocular classification of Retinoblastoma, in completed patients clinical data, unknown vital status and only 5 enucleated eyes’ tissues was performed the immunohistochemical analysis as a result making the impact to quality of research.
The diagnosis was made clinically before 2001 by using only B Scan, since 2001 and 2006 the computed axial tomography scanning of orbits and brain and magnetic resonance imaging was introduced respectively. Selective ophthalmic arterial infusion was also not available at our center. Furthermore, retinoblastoma is the paramount example of multidisciplinary care in pediatric cancer, and in contrast to other malignancies, it is not possible to advance in the treatment of this disease without the participation of multiple specialists, usually difficult to achieve even in developed countries.
In developing countries, poor education, lower socioeconomic conditions, and inefficient health care systems result in delayed diagnosis and suboptimal care. Furthermore, the complexity of multidisciplinary care required is seldom possible. While ocular salvage is a priority in the Western world, death from retinoblastoma is still a major problem in developing countries.
In Conclusion, Mongolian patients from rural areas are more frequently diagnosed at late stages showing the importance of regular screening program among 0-3 aged children for early detection of the tumor. Most Mongolian children whose retinoblastoma is diagnosed initially present with leukocoria detected by a parent, because routine pediatric screening for leukocoria via the red reflex test is not widely used in remote area.
We need to detect early stage of retinoblastoma in order to increase survival rate, ocular survival and preserve vision, establish good modern different type of treatment and create Mongolian guidelines for Retinoblastoma care. The implementation of International classification of RB, systemic intravenous chemotherapy and laser treatment for retinoblastoma, shows favorable outcome in the treatment of RB and further prognosis.
References
- Shields JA, S.C.R., Intraocular Tumors. Philadelphia (2008): 293-365.
- Ramasubramanian ASC. Epidemiology and magnitude of the problem. (2012).
- Shields CL and Shields JA. “Retino blastoma management: advances in enucleation, intravenous chemoreduction, and intra-arterial chemotherapy”. Current Opinion in Ophthalmology 21.3 (2010): 203-212.
- Shields CL and Shields JA. “Basic understanding of current classification and management of retinoblastoma”. Current Opinion in Ophthalmology 17.3 (2006): 228-234.
- Ramasubramanian A, S.C., Retinoblastoma. New Delhi, India. (2012): 70-78.
- Zhao J., et al. “Clinical presentation and group classification of newly diagnosed intraocular retinoblastoma in China”. British Journal of Ophthalmology 95.10 (2011): 1372-1375.
- Tsengelmaa C and M. “Altankhuu, Retinoblastoma in State Research Centre on Maternal & Children Health: Prevalence, Clinical and Survival Characteristics 1987-2005". The East Asian Forum, Program and Abstracts (2005): 59-60.
- Ozkan A., et al. “Retinoblastoma in Turkey: survival and clinical characteristics 1981-2004”. Pediatrics International 48.4 (2006): 369-373.
- Bonanomi MT., et al. “Retinoblastoma: a three-year-study at a Brazilian medical school hospital”. Clinics (Sao Paulo) 64.5 (2009): 427-434.
- Abramson DH., et al. “Presenting signs of retinoblastoma”. Journal of Pediatrics 132. (3 pt 1) (1998): 505-508.
- Song JS LJn and Lee TW. “Treatment and prognosis of retinoblastoma; clinicopathologic analysis of 101 cases”. Journal of the Korean Ophthalmological Society 39 (1998): 393-405.
- Owoeye JF., et al. “Retinoblastoma--a clinico-pathological study in Ilorin, Nigeria”. African Journal of Health Sciences 13 (1-2) (2006): 117-123.
- Kao LY., et al. “Retinoblastoma in Taiwan: survival and clinical characteristics 1978-2000”. Japanese Journal of Ophthalmology 46.5 (2002): 577-580.
- Rai P SI., et al. “Too late presentation of 53 patients with retinoblastoma: a big challenge. International Journal of Ophthalmology 9.2 (2009): 221-230.
- Badhu B., et al. “Clinical presentation of retinoblastoma in Eastern Nepal”. Clinical & Experimental Ophthalmology 33.4 (2005): 386-389.
- Patikulsila P. Retinoblastoma at Maharaj Nakorn Chang mai hospital; A 7- year study. Changmai Med Bull 40.4 (2001): 167-172.
- Sahu S., et al. “Retinoblastoma: problems and perspectives from India”. Pediatric Hematology Oncology Journal 15.6 (1998): 501-508.
- Berman EL., et al. “Outcomes in retinoblastoma, 1974-2005: the Children's Hospital, Westmead”. Clinical & Experimental Ophthalmology 35.1 (2007): 5-12.
- Chantada G., et al. “Late diagnosis of retinoblastoma in a developing country”. Archives of Disease in Childhood 80.2 (1999): 171-174.
- Reddy SC and S Anusya. “Clinical presentation of retinoblastoma in Malaysia: a review of 64 patients”. International Journal of Ophthalmology 3.1 (2010): 64-68.
- Sun XL., et al. “Immunohistochemical studies of retinoblastoma”. Japanese Journal of Ophthalmology 34.2 (1990): 149-157.
- Karim MM., et al. “Retinoblastoma: clinical and immunocytochemical observations”. Kobe Journal of Medical Sciences 42.3 (1996): 151-161.
- Yuge K., et al. “Immunohistochemical features of the human retina and retinoblastoma”. Virchows Archiv 426.6 (1995): 571-575.
- Xu KP., et al. “Immunohistochemical evidence of neuronal and glial differentiation in retinoblastoma”. British Journal of Ophthalmology 79.8 (1995): 771-776.
- Kashyap S., et al. “A histopathologic analysis of eyes primarily enucleated for advanced intraocular retinoblastoma from a developing country”. Archives of Pathology & Laboratory Medicine 136.2 (2012): 190-193.
Citation:
Tsengelmaa Chuluunbat., et al. “Retinoblastoma in Mongolia: Clinical Characteristics and Survival from 1987 to 2017”. Ophthalmology
and Vision Science 2.2 (2018): 230-240.
Copyright: © 2018 Tsengelmaa Chuluunbat., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.




































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.