Case Report
Volume 1 Issue 3 - 2017
White Glistening Dots in Macula: A Fundoscopy Clue for Genodermatosis
Department of Ophthalmology, Al Ameen Medical College and hospital, Bijapur, India
*Corresponding Author: Hosamani Sushma, Assistant Professor of Ophthalmology, Al Ameen Medical College and hospital, Bijapur,
India.
Received: August 03, 2017; Published: September 13, 2017
Abstract
Sjogren Larsson Syndrome(SLS), a traid of congenital icthyosis, mental retardation and spastic diplegia with bilateral macular dystrophy (seen in one third of cases and is pathognomic) was seen in a eight months baby and five year old children in two different Indian family born of consanguinous marriage. This case study is to emphasize the clinical importance of the ophthalmological features of the Sjögren-Larsson syndrome. Survey of available literature revealed around 200 SLS cases being reported.
Keywords: Sjogren Larsson Syndrome (SLS); Macular dystrophy; Congenital icthyosis; Spastic diplegia
Introduction
Sjogren Larsson Syndrome (SLS) is an autosomal recessive disorder characterised by congenital icthyosis, mental retardation and spastic diplegia/tetraplegia in addition a characteristic retinopathy which is reported in one third of these cases. SLS patients will have deficient activity of fatty aldehyde dehydrogenase (FALDH) [1]. Although no detailed epidemiological studies are available on incidence of SLS in India, we found only 10 such cases reported on web in India till today (one had macular dystrophy) but only few published in ophthalmic journals.
Case History
An 8 month girl (case 1) and 5year (case 2) old boy presented to us for ophthalmic evaluation. Patient gave history of generalized scaling of skin since birth and delayed milestones. History of consanguinity in parents was present. Both were term babies with approximate birth weight 2 kgs. There is no history of generalized tonic clonic seizures but parents were not sure of absence seizures. No dental/skeletal abnormality noted. Photophobia and conductive aphasia was present in case 2.
An 8 month girl (case 1) and 5year (case 2) old boy presented to us for ophthalmic evaluation. Patient gave history of generalized scaling of skin since birth and delayed milestones. History of consanguinity in parents was present. Both were term babies with approximate birth weight 2 kgs. There is no history of generalized tonic clonic seizures but parents were not sure of absence seizures. No dental/skeletal abnormality noted. Photophobia and conductive aphasia was present in case 2.
Cutaneous examination in both cases, revealed generalized scaling of skin of lamellar icthyosis type, pruritis though characteristic of SLS was not a complaint. Neurological examination revealed mental retardation and spastic diplegia (case 1). Muscle tone and brisk deep tendon reflexes in all four limbs were increased. Power in all four limbs was of grade 3/5. Fixed contracture at ankle and knee joint were noted. Ankle clonus was present.
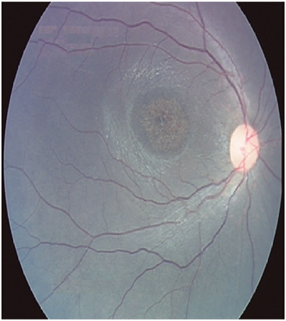
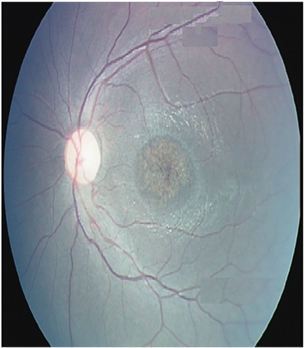
Ocular examination showed no abnormality in anterior segment. Visual acuity testing and fundus flourescein angiography could not be performed. Fundus examination revealed bilateral macular dystrophy in both cases with a characteristic bilateral glistening yellowish white crystalline deposits around macula (in case 2) and partial optic atrophy (in case 1).
MRI finding revealed bilateral cerebral atrophy with prominent sulci and subarchnoid space (in case 1). Delayed myelination (in case 2).
Discussion
Sjögren 1956; Sjögren and Larsson 1957 described a syndrome with following clinical features-congenital ichthyosis associated with spastic diplegia or tetraplegia (spastic pyramidal symptoms), aphasia, and low-grade dementia [1].
Very high prevalence of SLS has been observed in north east of Sweden where an incident of 8.3:100,000 births has been reported (Jagell., et al. 1981). However, a case has been reported from India are 10 (Kirubakaran., et al. 1982; Shrivastava., et al. 1986; Patki AH 1993; Sood., et al. 2002; 2 cases by Dhanuka AK 2002; Arvind Rup Singh 2002; S P Gupta 2011). Two sisters of Indian origin have also been reported from UK (Thakur and Smith 1991).
Skin changes will be in the form of icthyosis which is a generalized hyperkeratosis over trunk, joints, and the dorsal aspects of the hands and the feet. Pruritus is a prominent feature that is not found in other types of ichthyotic skin disorders [2].
Photophobia, macular dystrophy and decreased visual acuity are the most prominent ophthalmologic abnormalities and may be caused by accumulation of long-chain fatty alcohols or fatty aldehydes. These features are seen in one third of cases. [2]
There is usually spastic diplegia, occasionally tetraplegia, with mental retardation, epilepsy, and speech defects, dental, dermatological, skeletal, and retinal changes. Neurological component usually starts between four to thirty months and remains static after puberty [3].
The typical phenotype and clinical features of the SLS include congenital ichthysosis, lamellar-type hyperkeratosis, mental retardation, development delay, along with eye changes like pigmentary abnormality of macula (Gilbert., et al. 1968; Jagell., et al. 1981), juvenile macular dystrophy of retina (Willemsen., et al. 2000a), retinitis pigmentosa, chorioretinitis (Gilbert., et al. 1968), about 20% of the cases show glistening spots on the macula (Theile 1974), have also been reported.
Previous study reported that all patients exhibited bilateral, glistening yellow-white crystalline deposits that were located in the innermost retinal layers and appeared during the first 2 years of life. Repeated fundus photography in individual patients show that the dots became more numerous as the patients got older. Photophobia, subnormal visual acuity, myopia, and astigmatism were found in most of the patients [4].
Newborns usually manifest first ichthyosis, subsequently neurologic symptoms. Spasticity may be apparent before age three years and is more severe in the lower limbs than in other parts of the body [5].
The diagnosis should be considered in all patients with ichthyosis and central nervous system dysfunction. The presence of macular dystrophy and glistening white dots in the macular region is considered pathognomonic. This feature is present in one third of cases. The nature of the crystalline deposits in the retina is unclear. It is postulated that they might represent accumulations of long-chain fatty alcohols or fatty aldehydes [6-7].
In conclusion, Glistening white dots in macula are pathognomonic of SLS. Compared to previous studies as reported in literature, two years is the age at which the glistening white dots are seen in the macula (case 1 had no evident fundus findings compared to case 2 in this study). Limitation of this study was biochemical analysis. But on the typical clinical features and fundus findings it is reported as SLS and future management carried on. These patients needs follow up. But management in Sjogren Larsson Syndrome is supportive mainly to improve dermatological quality of life.
References
- Sjögren T and Larsson T. “Oligophrenia in combination with congenital ichthyosis and spastic disorders”. Acta Psychiatrica Et Neurologica Scandinavica 113 (1957): 1-112.
- Willemsen MA., et al. “Clinical, biochemical and molecular genetic characteristics of 19 patients with the Sjogren- Larsson syndrome”. Brain 124.7 (2001): 1426-1437.
- Dutra LA., et al. “Sjogren-Larsson syndrome: Case report and review of neurologic abnormalities and icthyosis”. Neurologist 15.6 (2009): 332-334.
- Willemsen MA., et al. “Juvenile macular dystrophy associated with deficient activity of fatty aldehyde dehydrogenase in Sjögren-Larsson syndrome”. American Journal of Ophthalmology 130.6 (2000): 782-789.
- Carney G., et al.“Sjögren-Larsson syndrome: seven novel mutations in the fatty aldehyde dehydrogenase gene ALDH3A2”. Human Mutation 24.2 (2004): 186.
- Willemsen MA., et al.“Juvenile macular dystrophy associated with deficient activity of fatty aldehyde dehydrogenase in Sjögren-Larsson syndrome. American Journal of Ophthalmology 130.6 (2000): 782-789.
- Gupta S P., et al.“Sjogren Larsson syndrome: A case report of a rare disease”. Indian Dermatology Online Journal 2.1 (2011): 31-33.
Citation:
Hosamani Sushma., et al. “White Glistening Dots in Macula: A Fundoscopy Clue for Genodermatosis”. Ophthalmology and Vision
Science 1.3 (2017): 114-118.
Copyright: © 2017 Hosamani Sushma., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.





































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.