Research Article
Volume 1 Issue 1 - 2017
Profile of Keratoconus in Selected Eye Clinics, Accra: A Retrospective Study
1Department of Optometry and Visual Science, Kwame Nkrumah University of Science and Technology (KNUST), Kumasi–Ghana
2Friends Eye Centre (Unite for Sight), Kumasi–Ghana
2Friends Eye Centre (Unite for Sight), Kumasi–Ghana
*Corresponding Author: Doreen Nelson-Ayifah, OD Teaching and Research Assistant, Department of Optometry and Vision Science, Kwame Nkrumah University of Science and Technology, PMB-Kumasi, Ghana.
Received: November 30, 2016; Published: March 11, 2017
Abstract
Background: Keratoconus is an ectatic corneal dystrophy characterized by conical bulging of the paracentral cornea with progressive thinning and scarring resulting in painless loss of vision. It is prevalent among all races with a prevalence of about 1 per 2000 in the general population. Very few studies have been conducted on keratoconus in African countries such as Ghana. The purpose of this study was to determine the profile of keratoconus in selected eye clinics in the Greater Accra Region of Ghana.
Method: Medical records of patients who visited the selected eye clinics from the year 2010 to 2015 were reviewed. Information on gender, age at diagnosis, place of residence, mode of referral, visual symptoms at the initial hospital presentation, keratometry readings, entrance visual acuity, management and best corrected visual acuity (BCVA) was recorded. Data was entered and analyzed using the Statistical Package for the Social Sciences (SPSS) version 21. Analysis was done at a 95% confidence level.
Results: A total of 78 medical records were reviewed. The condition was found to manifest in the early 20 and was more common and severe in males than females with a male to female ratio of 3:1. Most hospital referrals were done by optometrists with the most common visual symptom being reduced/blurred vision. Contact lenses improved vision the most, followed by spectacles and then penetrating keratoplasty (PKP).
Conclusion: Optical corrections (spectacles and contact lenses) continue to play a predominant role in the management of keratoconus as compared to penetrating keratoplasty.
Keywords: Keratoconus; Keratometry Readings; Visual Acuity; Reduced/Blurred Vision; Spectacles; Contact Lens; Penetrating Keratoplasty
Abbreviations: BCVA: Best Corrected Visual Acuity; VA: Visual Acuity; PKP: Penetrating Keratoplasty; K-readings: Keratometry Readings; RGP: Rigid Gas Permeable
Introduction
Keratoconus is an ectatic corneal dystrophy characterized by conical bulging of the paracentral cornea with progressive thinning and scarring resulting in painless loss of vision [1]. It usually begins at puberty and classically progresses until the third or fourth decades of life where there seem to be a reduction or halt in the progression of the disease [2]. The condition is mostly bilateral (85%) but not symmetrical [3]. The etiology of the condition and its progression is not well understood. However, genetic factors are considered fundamental to its development [4] as well as some factors including atopy, mechanical trauma as a result of chronic eye rubbing and chronic exposure to ultraviolet radiations [5-7]. Keratoconus patients have been found to present with symptoms such as distorted vision, poor visual acuity with spectacles, tearing and ocular allergy [8,9]. Diagnosis is usually made based on patient history together with some clinical signs revealed by keratometry and slitlamp examination. However, corneal topography is the most sensitive method for diagnosing keratoconus [7]. Optical corrections (spectacles and contact lenses) are the first line of treatment for the distorted vision caused by keratoconus while surgical modes of treatment are considered when management with optical corrections are unsuccessful [8]. Studies that have been conducted on corneal diseases in Ghana have focused mainly on infectious and inflammatory diseases with very little attention paid to non-inflammatory ectatic corneal diseases like keratoconus; in spite of the evidence of the prevalence of risk factors for keratoconus in Ghana [10-12]. This study determines the profile of keratoconus in selected eye clinics in the Greater Accra Region of Ghana - the demographic profile, presenting visual symptoms and the management and functional outcomes of keratoconus patients. To the authors’ best knowledge, this will be the first published data on keratoconus in Ghana, hence it will be useful information for eye health workers and researchers in Ghana and other places.
Methods
Three eye clinics in Accra known to treat patients with keratoconus were selected to be included in the study. However only two participated due to challenges in getting permission from the relevant authorities in one of the clinics. Medical records of all keratoconus patients who visited these clinics from the year 2010 to 2015 were reviewed. Data on gender, age at diagnosis, place of residence, mode of referral, visual symptoms at the initial hospital presentation, keratometry readings (K-readings), entrance visual acuity, management options given and the degree of visual success in terms of best corrected visual acuity (BCVA) was recorded. Visual acuity was recorded in the LogMAR notation. The data was entered and analyzed using the Statistical Package for the Social Sciences (SPSS) version 21. The participants were categorized into 4 different age groups - Group 1: < 20 years, Group 2: 20-29 years, Group 3: 30-39 years and Group 4: > 39 years. Analysis was done at a 95% confidence level.
Results
Demographic Profile
A total of seventy-eight keratoconus cases were recorded-fifty bilateral cases (64.10%) and twenty-eight unilateral cases (35.90%). Twenty of the unilateral cases affected the right eye while eight affected the left eye. The demographic information of patients is presented in Tables 1 and 2. The measurements reported in Table 2 are for the right eye only since One-way ANOVA did not reveal any significant difference between the mean entrance visual acuity (VA) for both eyes with respect to age groups (p = 0.215) and gender (p = 0.260). Additionally, the keratometry readings for both eyes in most bilateral cases were comparable and there were more right eye cases than left eye.
A total of seventy-eight keratoconus cases were recorded-fifty bilateral cases (64.10%) and twenty-eight unilateral cases (35.90%). Twenty of the unilateral cases affected the right eye while eight affected the left eye. The demographic information of patients is presented in Tables 1 and 2. The measurements reported in Table 2 are for the right eye only since One-way ANOVA did not reveal any significant difference between the mean entrance visual acuity (VA) for both eyes with respect to age groups (p = 0.215) and gender (p = 0.260). Additionally, the keratometry readings for both eyes in most bilateral cases were comparable and there were more right eye cases than left eye.
| Patient characteristic | Number | Percentage (%) |
| Mean age at initial visit Male Female |
22 ± 9.06 22.43 ± 8.68 20.91 ± 10.11 |
- |
| Mode of referral Optometrist Ophthalmologist Not Defined Self-reported |
37 10 12 19 |
47.44 12.82 15.38 24.36 |
| Refractive correction at initial visit Spectacles Contact lenses |
52
34 18 |
66.67 |
Table 1: The demographic profile of keratoconus patients as presented in Table 1.
| Gender Age Group (years) | ||||||
| Male | Female | < 20 | 20–29 | 30–39 | > 39 | |
| Number of subjects (%) | 56 (71.7%) | 22 (28.3%) | 33 (42.3%) | 33 (42.3%) | 8 (10.3%) | 4 (5.1%) |
| Entrance visual acuity (Mean ± SD) | 1.16 ± 0.53 | 1.00 ± 0.54 | 1.14 ± 0.56 | 1.07 ± 0.51 | 1.27 ± 0.64 | 1.00 ± 0.24 |
| Keratometry readings (Mean ± SD) | 56.00 ± 4.31 | 55.60 ± 2.64 | 55.75 ± 3.82 | 54.43 ± 4.38 | 57.06 ± 3.71 | 55.18 ± 3.85 |
Table 2: Measurement and distribution of keratoconus as shown in Table 2.
Presenting Visual Symptoms
The most common visual symptom reported was reduced/blurred vision while pain was the least presenting visual symptom (Table 3).
The most common visual symptom reported was reduced/blurred vision while pain was the least presenting visual symptom (Table 3).
| Symptoms | Number (N = 78) | Percentage (%) |
| Reduced/blurred vision | 78/78 | 100.00 |
| Itching | 68/78 | 87. 20 |
| Tearing | 47/78 | 60. 30 |
| Photophobia | 45/78 | 57. 70 |
| Poor acuity with spectacles | 28/78 | 35. 90 |
| Pain | 26/78 | 33. 30 |
Percentages are row percentage.
Table 3: Presenting visual symptoms as shown in Table 3.
Table 3: Presenting visual symptoms as shown in Table 3.
Hospital Management of Keratoconus
At the initial visit, some patients did not require a change in their existing refractive correction while others had their refractive correction changed on a later visit. Other patients received penetrating keratoplasty (PKP). Management of keratoconus was either optical (spectacles or contact lenses) or surgical (PKP). Twenty-three patients (29.49%) were managed with spectacles, thirty-four patients (43.59%) were fitted with contact lenses and twenty-one patients (26.92%) received PKP (Table 4). The main reason for patients undergoing PKP was due to their poor visual acuity with optical correction.
At the initial visit, some patients did not require a change in their existing refractive correction while others had their refractive correction changed on a later visit. Other patients received penetrating keratoplasty (PKP). Management of keratoconus was either optical (spectacles or contact lenses) or surgical (PKP). Twenty-three patients (29.49%) were managed with spectacles, thirty-four patients (43.59%) were fitted with contact lenses and twenty-one patients (26.92%) received PKP (Table 4). The main reason for patients undergoing PKP was due to their poor visual acuity with optical correction.
| Management option | Number (N = 78) | Percentage % |
| Optical correction Spectacles Contact lens Monocular fitting Binocular fitting |
57 23 34 11 23 |
73.08 |
| Penetrating keratoplasty Post-PKP requiring spectacles |
21 17 |
26.92 |
Table 4: Hospital management of keratoconus as shown in Table 4
Among patients who were managed with contact lenses, twenty-two (64.71%) were fitted with rigid gas permeable contact lenses, eight (23.53%) were fitted with full scleral lenses, three (8.82%) were fitted with semi-scleral lenses and one (2.94%) was fitted with keratoconus soft lens. Most of the patients (88.23%) wore their contact lenses for about seven hours a day and 11.77% wore their lenses between eight and twelve hours a day.
Management Outcomes
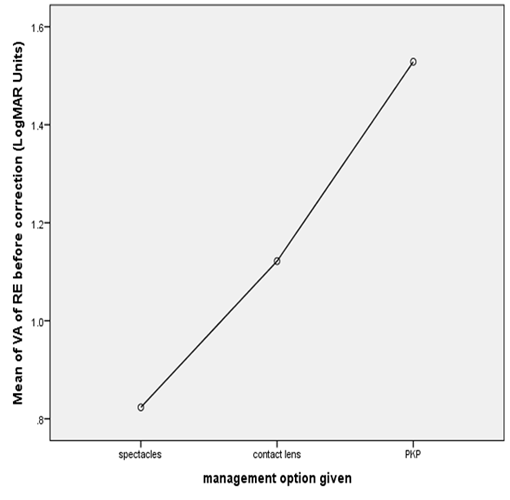
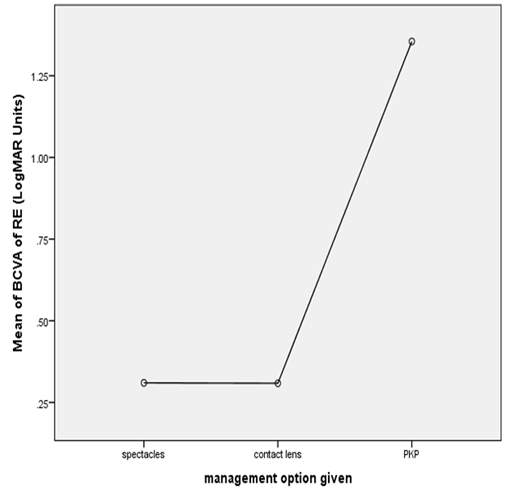
The outcome of the various management options is shown in Figures one and two. From the mean plots, the average entrance visual acuity of the right eye of patients who were managed with spectacles was 0.823 ± 0.490 LogMAR units. This improved to 0.309 ± 0.3246 LogMAR units.
The outcome of the various management options is shown in Figures one and two. From the mean plots, the average entrance visual acuity of the right eye of patients who were managed with spectacles was 0.823 ± 0.490 LogMAR units. This improved to 0.309 ± 0.3246 LogMAR units.
The average entrance visual acuity of patients who were managed with contact lenses in the right eye was 1.122 ± 0.452 LogMAR units. This improved to 0.310 ± 0.3699 LogMAR units.
The average entrance visual acuity of patients who were managed with PKP in the right eye was 1.529 ± 0.393 LogMAR units. This improved to 1.355 ± 0.4872 LogMAR units.
One-way ANOVA revealed a statistically significant difference between the mean BCVA for the various management options (F = 51.469, p = 0.0001). Post Hoc tests (Tukey HSD and LSD) showed no statistically significant difference between the mean BCVA from spectacles and contact lenses (p = 0.990). However, the difference between the mean BCVA from the optical corrections (spectacles and contact lenses) and PKP was found to be statistically significant (p = 0.0001).
Discussion
Demographic Profile of Patients
Age
Age plays a role in the onset, progression and arrest of the progression of keratoconus. A number of authors have stated an average age of onset for keratoconus; some of which include an early age of 14 years [13] and a much later age of 30 years [14]. In the present study, it was not possible to determine the mean age of onset because most of the patients (75.64%) had already been diagnosed with keratoconus and been managed by their eye health professionals for some time before they were referred to the selected eye clinics. The mean age at initial visit to the selected eye clinics was however found to be 22 ± 9.06. A previous study found the mean age at hospital referral to be 28years [15]. The difference in these findings could be due to the different ages at which keratoconus patients were referred. Most of the patients (84.62%) in this study were aged below thirty. Hence, this study supports the earlier reports that keratoconus usually begins at puberty and may progress until the third decade of life [2,3,13]. This finding emphasizes the need for early detection and management in the younger population since early detection and appropriate management may improve the quality of life of keratoconus patients [17].
Age
Age plays a role in the onset, progression and arrest of the progression of keratoconus. A number of authors have stated an average age of onset for keratoconus; some of which include an early age of 14 years [13] and a much later age of 30 years [14]. In the present study, it was not possible to determine the mean age of onset because most of the patients (75.64%) had already been diagnosed with keratoconus and been managed by their eye health professionals for some time before they were referred to the selected eye clinics. The mean age at initial visit to the selected eye clinics was however found to be 22 ± 9.06. A previous study found the mean age at hospital referral to be 28years [15]. The difference in these findings could be due to the different ages at which keratoconus patients were referred. Most of the patients (84.62%) in this study were aged below thirty. Hence, this study supports the earlier reports that keratoconus usually begins at puberty and may progress until the third decade of life [2,3,13]. This finding emphasizes the need for early detection and management in the younger population since early detection and appropriate management may improve the quality of life of keratoconus patients [17].
It was expected that older patients would present with higher K-readings due to progression of the disease. However, there was no association between the age of patients and the mean K-readings. This finding suggests that age may not be a factor in determining the severity of the disease as the disease could remain stationary at its first appearance or progress over a period of time [16]. This finding is consistent with a previous study conducted in Malaysia [17].
Gender
Awareness of gender-based differences is important in prevention, diagnosis and management of conditions that may be more prevalent to one gender. The reported gender ratios vary for keratoconus. Some authors have reported a higher incidence among females [18,19] while others have reported a higher incidence among males [8, 20-22] with an average male to female ratio of 3:2 [22]. In the present study, there was a higher incidence in males with a male to female ratio of 3:1 which is comparable to the ratio found by Weed [21] and Thalainen [22]. Although many studies have shown a male dominance for keratoconus, the fact that the condition is more common in males remains modest and it is quite difficult to conclude on a gender dominance for keratoconus [1].
Awareness of gender-based differences is important in prevention, diagnosis and management of conditions that may be more prevalent to one gender. The reported gender ratios vary for keratoconus. Some authors have reported a higher incidence among females [18,19] while others have reported a higher incidence among males [8, 20-22] with an average male to female ratio of 3:2 [22]. In the present study, there was a higher incidence in males with a male to female ratio of 3:1 which is comparable to the ratio found by Weed [21] and Thalainen [22]. Although many studies have shown a male dominance for keratoconus, the fact that the condition is more common in males remains modest and it is quite difficult to conclude on a gender dominance for keratoconus [1].
Gender and Severity of Keratoconus
In this study, two measurements were assumed to be indicators of the severity of keratoconus-the entrance visual acuity and the K-readings; owing to the fact that the more advanced the keratoconus, the poorer the vision and the higher the k-readings because VA decreases as corneal curvature and astigmatism increase. The study sought to find out if there were any gender differences with respect to the severity of the condition. There was no significant difference between the entrance VA (p = 0.267) of males and females; however, males were likely to have a higher K-reading than females (p = 0.027). Although the entrance VA may give an idea of the severity of the condition, it may not be a reliable indicator. Asiri and colleagues reported a weak correlation between entrance VA and the severity of keratoconus because of the variable influence of the amount, regularity, and obliqueness of the astigmatism, the level of progressive myopia, the scar type, morphology of the cone, and extent of any atopic disease [9]. K-readings nevertheless remain a more reliable indicator of the severity of the condition [5]. Hence, it can be postulated from the results obtained from this study that gender could influence the severity of keratoconus; with males having a higher level of severity than females. This is probably due to the fact that more males are affected at an earlier age than females. This finding is consistent with the results obtained by Owen and Gamble in their study on the Profile of Keratoconus in New Zealand. They found that men have an earlier onset of keratoconus and a more rapid disease course [20]. However, some authors found no significant difference in the disease severity as determined by K-readings and gender [17, 23].
In this study, two measurements were assumed to be indicators of the severity of keratoconus-the entrance visual acuity and the K-readings; owing to the fact that the more advanced the keratoconus, the poorer the vision and the higher the k-readings because VA decreases as corneal curvature and astigmatism increase. The study sought to find out if there were any gender differences with respect to the severity of the condition. There was no significant difference between the entrance VA (p = 0.267) of males and females; however, males were likely to have a higher K-reading than females (p = 0.027). Although the entrance VA may give an idea of the severity of the condition, it may not be a reliable indicator. Asiri and colleagues reported a weak correlation between entrance VA and the severity of keratoconus because of the variable influence of the amount, regularity, and obliqueness of the astigmatism, the level of progressive myopia, the scar type, morphology of the cone, and extent of any atopic disease [9]. K-readings nevertheless remain a more reliable indicator of the severity of the condition [5]. Hence, it can be postulated from the results obtained from this study that gender could influence the severity of keratoconus; with males having a higher level of severity than females. This is probably due to the fact that more males are affected at an earlier age than females. This finding is consistent with the results obtained by Owen and Gamble in their study on the Profile of Keratoconus in New Zealand. They found that men have an earlier onset of keratoconus and a more rapid disease course [20]. However, some authors found no significant difference in the disease severity as determined by K-readings and gender [17, 23].
Mode of Referral
Of the fifty-nine hospital referrals, 62.71% were done by optometrists which is probably because optometrists are primary eye care professionals in Ghana and so are usually the first point of call for most keratoconus patients as a result of the earlier report of reduced/blurred vision. It may also be due to the fact more optometrists practice in private eye clinics/optical shops in Ghana (compared to other cadres of eye health) where patients are likely to present first with symptoms of blurred vision. A similar finding has been reported by other authors [8,21].
Of the fifty-nine hospital referrals, 62.71% were done by optometrists which is probably because optometrists are primary eye care professionals in Ghana and so are usually the first point of call for most keratoconus patients as a result of the earlier report of reduced/blurred vision. It may also be due to the fact more optometrists practice in private eye clinics/optical shops in Ghana (compared to other cadres of eye health) where patients are likely to present first with symptoms of blurred vision. A similar finding has been reported by other authors [8,21].
Presenting Visual Symptoms
The symptoms reported in this study have been reported by some authors [7,8,20,21]. Reduced/blurred vision accounted for the most common visual symptom because it is usually one of the first noticeable symptoms for most keratoconus patients due to the irregular astigmatism and progressive myopia caused by the disease. A higher percentage (87.20%) of the patients complained of itching probably be due to the association between keratoconus and atopic disorders which causes the release of histamine during allergic episodes resulting in eye itchiness. Allergic conjunctivitis has been reported as one of the common outpatient eye conditions in most eye clinics in Ghana due to the environmental conditions in the country [24]. Previous studies have also reported an association between chronic eye itching and keratoconus which was attributed to atopy [7,25,26].
The symptoms reported in this study have been reported by some authors [7,8,20,21]. Reduced/blurred vision accounted for the most common visual symptom because it is usually one of the first noticeable symptoms for most keratoconus patients due to the irregular astigmatism and progressive myopia caused by the disease. A higher percentage (87.20%) of the patients complained of itching probably be due to the association between keratoconus and atopic disorders which causes the release of histamine during allergic episodes resulting in eye itchiness. Allergic conjunctivitis has been reported as one of the common outpatient eye conditions in most eye clinics in Ghana due to the environmental conditions in the country [24]. Previous studies have also reported an association between chronic eye itching and keratoconus which was attributed to atopy [7,25,26].
Tearing was the third most common symptom reported by patients in this study. This is probably due to a disorder in tear quality caused by the disease as found by Dogru., et al. [27] and Acera [28]. The report of photophobia may be due to damage to the ocular surface caused by the disease.
As keratoconus progresses, the degree of myopia and irregular astigmatism increases such that a patient may not be satisfied with the vision provided by their current prescription. About a third (35.90%) of the patients reported poor acuity with their spectacle prescription due to the change in degree of refractive error as the condition progresses. The fewer number of patients presenting with this symptom could be attributed to the fact that only thirty-four patients had spectacle prescription at the time of initial visit.
Pain is usually experienced by patients with advanced form of the disease. The pain experienced is mostly due to acute corneal hydrops - a painful condition characterized by stromal edema due to leakage of aqueous through a tear in descemet membrane. Only 33.33% patients presented with pain which could mean that they had an advanced form of the condition that could have resulted in the formation of acute corneal hydrops; causing pain.
Management of Keratoconus and Their Outcomes
A wide range of management options are available for the management of keratoconus; however, the options prescribed for the patients in this study were spectacles, contact lenses and PKP.
A wide range of management options are available for the management of keratoconus; however, the options prescribed for the patients in this study were spectacles, contact lenses and PKP.
Contact lenses remain the most cost effective mode of treatment for keratoconus [8,29]. This was confirmed in the present study as most of the patients (43.59%) were managed with contact lenses. The average improvement in visual acuity of the right eye of these patients was 0.823 LogMAR units which is equivalent to approximately eight lines on the visual acuity chart.
A wide range of contact lens types exist for managing keratoconus with rigid gas permeable (RGP) lenses being the most dispensed. In the present study, patients (64.71%) who received contact lenses were managed with RGP lenses which is comparable to the study by Lim and Vogt’s [8]. Patients who could not tolerate RGP lenses were given soft lenses, scleral and semi-scleral for comfort as scleral lenses have been found to provide acceptable visual acuity and comfort in patients with keratoconus [30].
A good number of patients (29.49%) were managed with spectacles which may be an indication that these patients had mild keratoconus since spectacles can only improve vision in the early stages of the disease. Spectacles provided an improvement in visual acuity of 0.452 LogMAR units which is equivalent to approximately five lines.
The indication for PKP found in this study was failure of optical corrections to give good visual acuity; hence most patients who underwent PKP had advanced form of the disease.
The 26.92% of patients who had undergone PKP is consistent with finding from Zadnik., et al. [14]. The need for contact lens wear after PKP has been reported to range from as low as 19% [21] to as high as 60% [31]. In the present study, 80.95% of patients who underwent PKP were given spectacles since the eye clinic where the surgeries were done did not have a contact lens clinic. The higher percentage of patients requiring spectacles post-PKP in this study could be as a result of the lower visual acuity (1.355 ± 0.4872 LogMAR units) outcome of the surgeries.
Analysis of variance and post hoc testing gave no significant differences between the average BCVA of spectacles and contact lenses which means that spectacles remain effective in improving VA in mild cases while contact lenses improve VA in moderate to severe cases of keratoconus. A significant difference was found in the average BCVA of optical corrections and PKP which confirms the fact that PKP does not improve VA in keratoconus better than optical corrections.
Acknowledgement
We are grateful to the management and staff of the eye clinics which were involved in the study.
We are grateful to the management and staff of the eye clinics which were involved in the study.
Declarations
a. Conflict of Interest
NA
a. Conflict of Interest
NA
b. Ethical Approval
Approval was sought from the Committee for Human Research Publication and Ethics (KNUST) and the administrators of the various eye clinics concerning the procedures and protocols for this study.
Approval was sought from the Committee for Human Research Publication and Ethics (KNUST) and the administrators of the various eye clinics concerning the procedures and protocols for this study.
References
- Adel B. “Textbook on Keratoconus: New Insights”. Jaypee Brothers, Medical Publishers Pvt. Limited New Delhi, India (2011): pp 3.
- The American Academy of Optometry. [Cited 2015 Sept 18];
- Khurana AK. “Comprehensive Ophthalmology, Fourth Edition”. New Age International (P) Publishers New Delhi (2007): Pp 119-120.
- Sugar J and Macsai MS. “What Causes Keratoconus?” Cornea 31.6 (2012): 716-719.
- Romero-Jimenez M., et al. “Keratoconus: A Review”. Contact Lens and Anterior Eye 33.4 (2010): 157-166.
- McMonnies CW. “Mechanisms of Rubbing-Related Corneal Trauma in Keratoconus”. Cornea 28.6 (2009): 607-615.
- Gordon-Shaag A., et al. “The Epidemiology and Etiology of Keratoconus”. International Journal of Keratoconus and Ectatic Corneal Disorders 1.1 (2012): 7-15.
- Lim N and Vogt U. “Characteristics and Functional Outcomes of 130 Patients with Keratoconus Attending a Specialist Contact Lens Clinic”. Eye 16.1 (2002): 54-59.
- Assiri AA., et al. “Incidence and Severity of Keratoconus in Asir Province, Saudi Arabia”. British Journal of Ophthalmology 89.11 (2005): 1403-1406.
- Hogewoning A., et al. “Skin Diseases among Schoolchildren in Ghana, Gabon and Rwanda”. International Journal of Dermatology 52.5 (2013): 589-600.
- Amoah AS., et al. “A Review of Epidemiological Studies of Asthma in Ghana”. Ghana Medical Journal 46.2 Suppl (2012): 23-28.
- Addo-Yobo E., et al. “Risk Factors for Asthma in Urban Ghana”. Journal of Allergy and Clinical Immunology 108.3 (2001): 363-368.
- Li X., et al. “Longitudinal Study of Normal Eyes in Unilateral Keratoconus Patients”. Ophthalomology 111.3 (2004): 440-446.
- Zadnik K., et al. “Biomicroscopic Signs and Disease Severity in Keratoconus”. Cornea 15.2 (1996):139-46.
- Crews MJ., et al. “The Clinical Management of Keratoconus: A 6 Year Retrospective Study”. CLAO 20.3 (1994): 194-197.
- Olivares Jiminez L., et al. “Keratoconus: Age of Onset and Natural History”. Optometry and Vision Science 74.3 (1997): 147-151.
- Mohd-Ali B., et al. “Clinical Characteristics of Keratoconus Patients in Malaysia: A Review from a Cornea Specialist Centre”. Journal of Optometry 5.1 (2012): 32-42.
- Thomas CI. “The Cornea”. CC Thomas: Springfield and Illinois (1955): 233–244.
- Barth J, Statistik U, Keratokonusfaelle M and Befallenden A MD Thesis, University of Zurich. 1948.
- Owens H and Gamble G. “Profile of Keratoconus in New Zealand”. Cornea 22.2 (2003): 122–125.
- Weed KH and McGhee CNJ. “Referral Patterns, Treatment, Management and Visual Outcome in Keratoconus”. Eye 12.Pt4 (1998): 663-668.
- Thalainen A. “Clinical and epidemiological features of keratoconus genetic and external factors in the pathogenesis of the disease”. Acta Ophthalmologica 178 (1986): 1–64.
- Fink BA., et al. “Differences in Keratoconus as a Function of Gneder”. American Journal of Ophthalmology 140.3 (2005): 459-468.
- Ghana Health Service (2013). Eye Health Systems assessment (EHSA): Ghana Country Report.
- Krachmer JH., et al. “Keratoconus and Related Non-inflammatory Corneal Thinning Disorders”. Survey of Ophthalmology 28.4 (1984): 293-322.
- Bawazeer AM., et al. “Atopy and Keratoconus: A Multivariate Analysis”. British Journal of Ophthalmology 84.8 (2000): 834-836.
- Dogru M., et al. “Tear Function and Ocular Surface Changes in Keratoconus”. Ophthalmology 110.6 (2003): 1110-1118.
- Acera A., et al. “Changes in Tera Protein Profile in Keratoconus Disease”. Eye 25.9 (2011): 1225-1233.
- Lass J., et al. “Clinical Management of Keratoconus: A Multicenter Analysis”. Ophthalmology 97.4 (1990): 433-445.
- Schornack M and Patel S. “Scleral Lenses in the Management of Keratocnus”. Eye and Contact Lens Science and Clinical Practice 36.1 (2010): 39-44.
- Smiddy WE., et al. “Keratoconus: Contact Lens or Keratoplasty”. Ophthalomology 95.4 (1989): 487-492.
Citation:
Doreen Nelson-Ayifah., et al. “Profile of Keratoconus in Selected Eye Clinics, Accra: A Retrospective Study”. Ophthalmology and Vision Science 1.1 (2017): 8-16.
Copyright: © 2017 Doreen Nelson-Ayifah., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.