Case Report
Volume 3 Issue 5 - 2018
A Cost-effective Method to Establish Occlusal Guidances, in the Pre-Doctoral Setting
1BDS, DDS, DICOI, NYUCD Clinical Instructor, New York, USA
2DDS, NYUCD ’15, New York, USA
2DDS, NYUCD ’15, New York, USA
*Corresponding Author: Maged Iskaros, BDS, DDS, DICOI, NYUCD Clinical Instructor, New York, USA.
Received: July 22, 2018; Published: August 06, 2018
The subject of occlusal rehabilitation has generated substantial dental literature.A review of the literature provides multiple recommendations to provide a functional and optimal standard of care when modifying or establishing occlusal scheme in a patient.
Most practitioners understand that developing an appropriate occlusion for a patient involves developing occlusal guidance individual to each patient. [1-3] This consists of multiple points of guidance and multiple guidance schemes such as incisal guidance with canine protected occlusion, or group function, or an occlusal scheme void of any healthy relationship. Therefore, when referring to a specific occlusal scheme, it should be noted that multiple guidance’s could be present.
Clark., et al. provides insight that there is not a single, universal criteria that denote an ideal functional occlusion. There is neither evidence for nor against establishing canine protected occlusion in patients. [2] However, the anatomy location, and functionality of the canine make them an ideal restorative tool.
- The canine has a good crown: root ratio, capable of tolerating high occlusal forces;
- The canine root has a greater surface area than adjacent teeth, providing greater proprioception
- The shape of the palatal surface of the upper canine is concave and is suitable for guiding lateral movements. [2]
- A fourth reason is that the canine plays a pivotal role in the crossover movement (extreme lateral – protrusive) and protects the four incisors.
Additionally, in 1983, it was determined by Williamson and Lundquist, via electromyographic activity, that the muscles of mastication were shown to be at rest during canine guidance more than during group function, suggesting that canine protected occlusion reduces muscle strain. [4]
While discussing potential occlusal schemes, Rinchuse., et al. state that those with a malocclusion, regardless of any change in occlusal scheme, the masticatory pattern remains the same. Therefore, those with a vertical chewing pattern would benefit from canine protected occlusion because it would allow for a sharp disocclusion while chewing. Whereas, those with a more flat or horizontal masticatory pattern could benefit from the stability offered by a group function pattern and the protection from the masticatory forces. [1]
Wiens., et al. provides a discussion on occlusal equilibration. The definition of occlusal equilibration is,” The elimination] of prematurities or deflective occlusal contacts or [creating] harmonious gliding tooth contacts, which reduces off-axis loading or atypical wear patterns.” [3] Specifically, on those patients who are symptomatic or those who will be undergoing. They also argue for a mutually protected occlusion and that the goal of occlusal therapy is to create stability and harmony by which ever means is appropriate for the patient in each specific case. There should not be any balancing interfering contacts during any movements in all cases in a natural and prosthetic dentition. Wiens., et al. also included support for a canine protected occlusion because of its effectiveness in eliminating occlusal interferences during laterotrusive, mediotrusive and protrusive excursions. [3]
Case Report
Patient KG, a 45 year old female, presented with moderate tooth decay, complaint of temporal tension headaches, and polypharmacy. The patient’s chief concern was that she “needed to replace a crown #18 because food keeps getting stuck.” Her medical history was positive for anxiety and depression, post-traumatic stress disorder, temporal tension headaches, facial muscle tension, and facial muscle spasms that are being managed with medications and therapy sessions. The patient’s dental history consists of bi-annual cleanings, a fixed-bridge in the upper right quadrant, crowns in the lower left quadrant, and amalgam and composite restorations throughout her mouth. She also has a past history of comprehensive orthodontics and orthognathic surgery. The patient denies the use of alcohol or tobacco.
Upon an interview and occlusal evaluation consisting of photographs, diagnostic casts, and intra/extra oral exam, it was determined that the patient had a pathological parafunctional occlusion causing pain during mastication,and difficulty eating. Clinically, the patient presented with wear facets, and enamel wear on her posterior teeth and non-existent canine anatomy on the mandibular canines, with damaging posterior occlusal contacts during lateral excursive movements Treatment to Patient KG included the restoration of occlusal guidance starting with occlusal equilibration, and restoration of a mutually protected occlusion via canine guided protection using resin-composite restorations to establish adequate incisor guidance (Anterior guidance).
Casts were articulated in maximum intercuspation (centric occlusion, CO) and an occlusal scheme was fabricated in a diagnostic wax-up on the incisal edges of select anterior teeth. Canine protected occlusion was the occlusal scheme of choice.
Following both Wein., et al. [3] and Clark., et al. [2] canine protected occlusion provides the simplest and most efficient way to disclude the posterior dentition during lateral excursions. The wax will be replaced with resin on #6, 8, 9, 11, 22, 23, 24, 25, 26, and 27. Then a clear vacuum sucked down proform (splint) was fabricated on the newly created incisor guidance. Patient is to wear this splint before, during and after the treatment to protect the restoration during the deep programming phase through complete reprogramming the muscles and full tolerance by the patient to the new occlusal scheme.
Wiens., et al. states that before any restoration of occlusal guidance or quadrant restorations be completed, removal of parafunctional interferences is indicated. This ensures harmonious posterior contacts without the additional stress added to the teeth. [1-3]
Prior to treatment, vacuum formed, 1 mm essix matrices were fabricated. Posterior balancing was achieved by removing interferences during centric, lateral, and protrusive movements. Next, minor preparation (beveling and roughening) of the maxillary and mandibular incisors was performed to increase retentive surface area and to improve the esthetics of the composite restorations. Enamel etching with 37% Phosphoric acid and Optibond Solo Plus bonding agent applied, composite was placed into the incisal edges of the vacuum formed matrices, adapted to the teeth, and cured through the clear matrix. The restorations were contoured and polished. The patient was sent home with the matrices and was instructed to wear them while sleeping. Wearing the matrices at night offered additional protection to the restorations against any nighttime bruxism.
At the 3 week follow up appointment, additional support was added to protect the patient’s dentition. Canine stops were placed on the lingual surface of teeth #6 and #11 in order to contribute to a solid, balanced rest position, and provide a greater protection to the newly created anterior guidance. Because of the anatomy of the canine, it is well suited to support these additional occlusal forces. [1-3] New matrices were delivered with openings for the canine rest stops. At 4 months, the patient did not have any complaints and there were no necessary repairs to the restorations needed. In other words, a state of occlusal stability was achieved.
Outcome of treatment
The patient was very receptive to the treatment and reported a decrease in masticatory muscle pain. The patient independently reported improvement in her joint pain and elimination of her temporal tension headaches. The patient reports less upper lip tension and a decrease in muscle spasms as well. The restorations, after 4 months, were functionally and cosmetically intact.
The patient was very receptive to the treatment and reported a decrease in masticatory muscle pain. The patient independently reported improvement in her joint pain and elimination of her temporal tension headaches. The patient reports less upper lip tension and a decrease in muscle spasms as well. The restorations, after 4 months, were functionally and cosmetically intact.
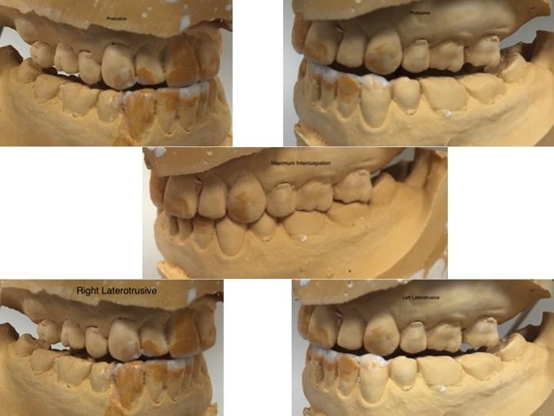
Figure 1: Diagnostic waxup, demonstrating maximum
intercuspation, protrusive, and laterotrusive movements.
Conclusion
Patient KG was not willing to immediately move to a definitive treatment modality without the option of test driving it first. Treating a patient following the protocol outlined above allows for a student dentist to learn the nuances of restoring a patient's traumatic occlusal scheme, while in a controlled setting. When restoring and establishing a new occlusal scheme, it has been shown that patients may develop temporomandibular disorder-like symptoms and an inability to adapt to a new situation [1]. With resin restorations, the risk of developing TMD symptoms is decreased.
Form and function go hand in hand. With this patient, her presenting condition resembled someone who does not have a stable occlusion or anterior guidance. By introducing the patient to a healthy occlusion, we were able to influence her function in a positive way by manipulating her form. With proper planning during the diagnosis stage, placement of composite became simple and easily managed during follow-up visits. The pre-treatment preparation by the student dentist was essential to a successful treatment modality because it allowed for a clear picture of the end goal of treatment. Treatment performed to Patient KG achieved beauty, longevity, form, function, and most importantly, stability.
References
- Rinchuse D., et al. “A contemporary and evidence-based view of canine protected occlusion”. American Journal of Orthodontics and Dentofacial Orthopedics132.1 (2015): 90-102.
- Clark JR and Evans RD. “Functional Occlusion: I. A Review”. Journal of Orthodontics 28.1 (2001): 76- 81.
- Wiens J., et al. “Occlusal Stability”. Dental Clinics of North America 58.1 (2014): 19-43.
- Williamson EH and Lundquist DO. “Anterior guidance: its effect on electromyographic activity of the temporal and masseter muscles”. Journal of Prosthetic Dentistry 49.6 (1983): 816-823.
Citation:
Maged Iskaros and Michael Hoglund. “A Cost-effective Method to Establish Occlusal Guidances, in the Pre-Doctoral Setting”.
Oral Health and Dentistry 3.5 (2018): 725-729.
Copyright: © 2018 Maged Iskaros and Michael Hoglund. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.





































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.