Case Report
Volume 2 Issue 3 - 2018
Alternate way to treat Ventriculo-Peritonitis
1Associate Professor, Assistant Registrar, Department of Neurosurgery, Bangladesh Medical College Hospital, Dhaka- 1209, Bangladesh
2Resident Assistant Professor, Department of Surgery, Bangladesh Medical College Hospital, Dhaka- 1209, Bangladesh
3Student, Bachelor of Medical Science Specializing in Pathology, Charles Sturt University, Wagga Wagga, 2678, Australia
2Resident Assistant Professor, Department of Surgery, Bangladesh Medical College Hospital, Dhaka- 1209, Bangladesh
3Student, Bachelor of Medical Science Specializing in Pathology, Charles Sturt University, Wagga Wagga, 2678, Australia
*Corresponding Author: Rezina Hamid, Associate Professor, Department of Neurosurgery, Bangladesh Medical College Hospital, Dhaka, Bangladesh.
Received: September 06, 2018; Published: September 19, 2018
Abstract
In Bangladesh Medical College we managed 3 male kids with venrticulo peritonitis. All of them came with infected shunts, abdominal distension, impaired conscious level and severe headache. They were treated with immediate shunt removal, ventricular drainage, instillation of intra ventricular and intra peritoneal antibiotics. Finally, after eradication of these infections all were given Ventriculo Peritoneal Shunts. Throughout the period nutritional imbalance was addressed aggressively.
Key Words: Shunt infection; Intra ventricular antibiotics; Intra peritoneal antibiotics
Abbreviations: CSF: Cerebrospinal Fluid; VPS: Ventriculo-Peritoneal Shunt; ETV: Endoscopic Third Ventriculostomy; CT: Computed Tomograph; IVT: Intra Ventricular Therapy; IP: Intraperitoneal; IV: Intravenous; G.C.S: Glasgow coma scale; USG: Ultrasonogram
Introduction
Hydrocephalus occurs when there is an excess production or, more commonly, decreased absorption of C.S.F, which might be a consequence of aqueductal stenosis resulting from meningitis, intracranial hemorrhage or brain tumor [1]. These morbid conditions are treated most commonly by VPS. ETV is done in some centers. ETV when successful, saves the patients from life threatening hazards of shunt complications. VPS is a bypass of accumulated CSF to the peritoneum, and through this huge absorptive surface, CSF ultimately reaches to blood. Though it is the most common neurosurgical procedure done for treating hydrocephalus, it bears a risk of malfunction and infection. The peritoneal end of the shunt tube may cause infection, pseudocyst formation, bowel perforation, abdominal abscess etc. Among them shunt infection was the most common [2]. Previously shunt infection rate was quite high (15-39%); but during the past two decades it dropped down to 2-9% [3]. Shunt infection is a dangerous condition. It increases the morbidity and mortality of the affected patients. Standard protocol to deal the infection is to remove the infected hardware, systemic antibiotics. External ventricular drainage is initiated to combat increased intra cranial pressure.
Some surgeons use Ommaya reservoir, which is placed in ventricle that draws CSF for drainage purpose (Figure 1a). IVT antibiotics are instilled through this route and directly to CSF. Being blood brain barrier, CSF penetration by antibiotics is poor. When a channel is made to the peritoneum, direct instillation of antibiotics can be done (Figure 1b). The Patient who develop peritonitis during peritoneal dialysis are frequently treated with IP antibiotics [4].
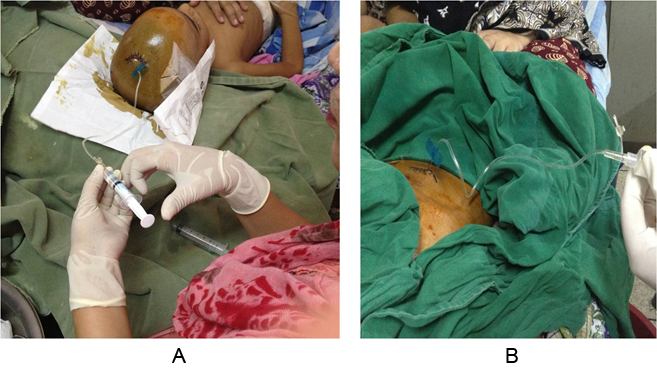
Figure 1: Intraventricular administration of Vancomycin through ommaya reservoir
& Intraperitoneal administration of Meropenum through ommaya reservoir.
Case Summary
Patient 1
A boy of 5 years was diagnosed with Idiopathic Congenital Hydrocephalus. He underwent VPS surgery in September 2015. Following month he was admitted with distended abdomen and severe vomiting. There was an infection in abdominal end of the tube. Exteriorization of abdominal end was done followed by revision. From October 15 to March 16 he underwent four revision surgeries. Throughout this period, he was treated by intravenous and oral antibiotics which included all generations of cephalosporins and carbapenum groups.
A boy of 5 years was diagnosed with Idiopathic Congenital Hydrocephalus. He underwent VPS surgery in September 2015. Following month he was admitted with distended abdomen and severe vomiting. There was an infection in abdominal end of the tube. Exteriorization of abdominal end was done followed by revision. From October 15 to March 16 he underwent four revision surgeries. Throughout this period, he was treated by intravenous and oral antibiotics which included all generations of cephalosporins and carbapenum groups.
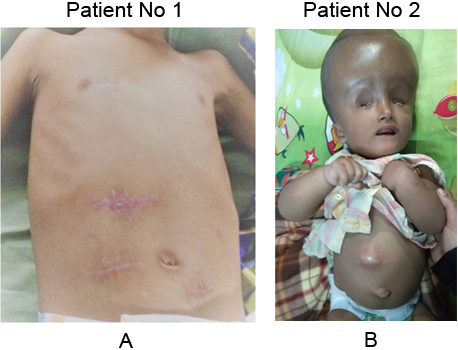
In 1st week of April 2016, he developed the same complains with severe headache and progressive loss of consciousness. With those problems he was referred to the Neurosurgery Department of Bangladesh Medical College Hospital. On admission we found an apathetic and emaciated boy with moderate anaemia, with an internal temperature of 102°F. Other features included was tense, tender abdomen and muscle guarding. There were 4 scar marks in the abdomen and 1 over the chest wall (Figure 2). Bowel sound was sluggish and no sign of pneumoperitoneum. He had G.C.S of 11 with signs of meningism. His blood count showed leucopenia, C reactive protein was high and an ultrasonogram of the abdomen revealed mild to moderate ascites. Plain X-ray showed no features of obstruction or perforation.
CT scan of the brain showed evidence of acute hydrocephalus, cranial end of shunt tube in situ. The provisional diagnosis was decided to be shunt malfunction (infection and obstruction).
On that very day removed the total shunt system was removed and sent for culture sensitivity. Two Ommaya reservoirs were placed, one in frontal horn of right lateral ventricle and another in the abdomen through a previous incision site. Immidiate after operation 30ml CSF was drawn 8 hourly followed by 1ml vancomycin daily, was instilled through intra ventricular route for 14 days. 250mg Meropenum was instilled through the peritoneal tube thrice (Figure 3). Shunt tube culture yieldedgrowth of Staphylococcus aureus sensitive to those drugs. On the 14th post operative day, when CSF yielded no growth and pleocytosis being resolved, he had definitive surgery of Endoscopic Third Ventriculostomy.After creating the stoma, the cistern was found to be scarred and the flow was very poor. Accordingly, a VPS was instilled and the ventricular and peritoneal catheters were removed. Post operatively he was maintained 7 days by IV Meropenum. On 9th post operative day, he was discharged with advice. He is on follow up, he returned to school after 6 months.
Patient 2
A baby boy of 1 year 4 months with history of previous shunt for hydranencephaly came with all signs of ventriculo peritonitis. He had a shiny reddish swelling over the epigastrium, neutrophilic leukocytosis,high fibrin degrading product, and USG showing an infected pseudocyst with multiple septa (Figure 2b). He was treated with immediate shunt removal, ommaya reservoir placement in ventricle, and drainage of the pseudocyst with peritoneal toileting. Around 200ml of thick pus was found in the cyst, with the rest of the abdomen not being involved. A drain was kept in situ, through which meropenum was given 8 hourly, with drain being clamped for half hour and then released.
A baby boy of 1 year 4 months with history of previous shunt for hydranencephaly came with all signs of ventriculo peritonitis. He had a shiny reddish swelling over the epigastrium, neutrophilic leukocytosis,high fibrin degrading product, and USG showing an infected pseudocyst with multiple septa (Figure 2b). He was treated with immediate shunt removal, ommaya reservoir placement in ventricle, and drainage of the pseudocyst with peritoneal toileting. Around 200ml of thick pus was found in the cyst, with the rest of the abdomen not being involved. A drain was kept in situ, through which meropenum was given 8 hourly, with drain being clamped for half hour and then released.
A culture of the shunt tube yielded no growth. Systemic, IP meropenum and IVT vancomycin was given for 14 days. Leucocytosis was resolved, fibrin degrading product were back to normal range and USG showed almost no residual cyst and collection. This neonate had a huge head with the cranial vault opened. Every day around 100 ml C.S.F was drained through the ommaya reservoir. He was discharged with VPS, Vitamin D and Acetazolamide at night, with latter given to minimize CSF production. After 6 months the patient found well and the cranial vault was almost closed. After 18 months of surgery, he expired from pneumonia.
Patient 3
This male child of 3 years came with h/o VPS. He had right sided hemiplegia, aphasia, fever, decreased level of consciousness, diffused abdominal distension and persistent vomiting. There was a continuous dribbling of clear fluid from a previous abdominal incision (Figure 2c). His CT scan showed sub dural hygroma and ventriculomegaly. USG showed no abdominal collection. The shunt was immediately removed, a 6 size feeding tube was put external ventricular drainage, and the sub dural collection was removed through a single burr hole. In the abdomen the fistulous tract was opened, saucerized and closed. A drain tube was inserted into the peritoneum. IVT Vancomycin , IP meropenum were initially prescribed but ceased when the culture of shunt tube showed profuse growth of pseudomonaus, and due to sensitivity of the previous antibiotics, the treatment was switched to colomycin. The patient received IV, IP and IVT colomycin in recommended dosage. The ventricular drainage was kept closed all times except to be opened 8 hourly.
This male child of 3 years came with h/o VPS. He had right sided hemiplegia, aphasia, fever, decreased level of consciousness, diffused abdominal distension and persistent vomiting. There was a continuous dribbling of clear fluid from a previous abdominal incision (Figure 2c). His CT scan showed sub dural hygroma and ventriculomegaly. USG showed no abdominal collection. The shunt was immediately removed, a 6 size feeding tube was put external ventricular drainage, and the sub dural collection was removed through a single burr hole. In the abdomen the fistulous tract was opened, saucerized and closed. A drain tube was inserted into the peritoneum. IVT Vancomycin , IP meropenum were initially prescribed but ceased when the culture of shunt tube showed profuse growth of pseudomonaus, and due to sensitivity of the previous antibiotics, the treatment was switched to colomycin. The patient received IV, IP and IVT colomycin in recommended dosage. The ventricular drainage was kept closed all times except to be opened 8 hourly.
At that time CSF was drained with the pressure gradient, and around 25ml of drainage brought back the pressure to normal. At the end of the procedure, IVT colomycin was given and the feeding tube was kept closed. After 14 days, the CSF culture became negative and leukocytosis was resolved, left sided VPS was given and ventricular and peritoneal drainage systems were removed. For next 7 days IV antibiotics were prescribed. The patient is in follow up for 3 months, he can utter words and stands with support.
Discussion
Children are most susceptible to shunt infections because of high level of skin bacterial concentration, immaturity of the immune system or more adherent types of bacteria. In a brief communication about ventriculo-peritoneal shunt infection, P Sargunas showed coagulase negative staphylococcus to be the most common isolated organism [5]. Skin commensals or direct wound contaminated cases correlated with gram positive shunt infections. Retrograde infection is another mechanism where asymptomatic perforation of bowel leading to retrograde progression of infection [6,7]. Jae-Joon Chung., et al. concluded that in various intra abdominal complications, secondary to ventriculo peritoneal shunt, infections were the most common consequence [7].
In the first case, the boy had a prolonged hospital stay. Culture of the shunt tube yielded growth of Staphylococcus Aureus. Though the second patient had huge pus in infected pseudocyst, no organism was detected. The third one was infected with pseudomonas.
All kids suffered abdominal complications. There was no visceral perforation or obstructions. Shunt infections correlate with increased risks of seizure, decreasing intellectual abilities and increase in mortality and morbidity rate [8]. After 6 months of the last surgery the kid started school. It will require more time to evaluate his neuro developmental status.
Mathew J., et al. stated that prior shunt infection with S. aureus or prolonged hospitalization were predictive for subsequent shunt infection with S.aureus. However they found that prior infection with coagulase negative Staphylococcus did not yield any predictive value. They concluded closer follow up that longer courses of treatment may be needed for patients with S. aureus shunt infection before planning a reinsertion procedure [9]. In this case, total duration of parenteral antibiotic therapy was 21 days.
IP meropenum is used to treat peritonitis in case of patients who have peritoneal dialysis. IP administration is superior to IV administration. Van Enday concluded IP administration of meropenum is well tolerated and safe [10]. P.J Vlaar., et al. suggested during peritonitis, bioavailability of IP meropenum is reasonably high [11].
In this case, the kidney function of the kids were perfect. As various studies showed intra peritoneum meropenum has high efficacy in treating peritonitis we created a port through a previous incision site. For last few months thepatient was getting full courses of IV and oral antibiotics ranging from all generation of cephalosporins, vancomycin and carbapenum. In spite of this and exteriorization of shunt he kept acquiring recurrent peritonitis.
Bangladesh is an under developed country and usually families affected by hydrocephalus fall marginally below the average socioeconomic status. They come from slum areas, broken families where nutrition and hygiene awareness is almost nil and so are very prone to shunt infections. As a part of treatment, the mother was taught about hygiene, hand washing and we arranged to feed the babies with high calorie food, especially rich in protein, fat and vitamins through the naso gastric tube to ensure adequate feeding to combat malnutrition and infection.
Conclusion
Ventriculoperitonitis and shunt obstructions result in high mortality and morbidity. Removal of infected hardware and IVT antibiotics are commonly used but in these cases IP antibiotics were used. They represent an innovative and fruitful method to treat shunt infection. It demands further study on pharmacokinetics of IP antibiotics. The role of proper nutrition and maintenance of hygiene play a crucial role in preventing and combating shunt infections along with aseptic surgery.
Declaration of competing Interests
The authors declare that they have no competing interests.
The authors declare that they have no competing interests.
Funding
We did not use any source of funding for the present work.
We did not use any source of funding for the present work.
Consent to publish
Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-chief of this journal.
Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-chief of this journal.
References
- Benjamin C., et al. “Post infectious hydrocephalus: the most common cause of Hydrocephalus; international federation for hydrocephalus and spina bifida, consultative status special category with economic and social council of the united nations consultative status, council of Europe.
- Jae-Joon Chung., et al. “Intraabdominal Complications Secondary to Ventriculoperitoneal shunts: CT Findings and Review of the Literature.” American journal of Roentgenology 193.5 (2009): 1311-1317.
- Crnich CJ safdar N and Maki DG: infections associated with imolanted medical devices. In Antibiotic and Chemotherapy. Anti-infective Agent and their use in Therapy 8th edition. Edited by: Finch RG, Greenwood D, Norrby SR, Whitley RJ Churchill. Livingstone; “(2003): 575-618.
- Philip Kam-Tao Li., et al. “Peritoneal Dialysis related Infections Recommendations: 2010 Update.” Journal of the International Society for Peritoneal Dialysis 30.4 (2010): 393-423.
- P Sarguna and V Lakshmi. “Ventriculoperitoneal shunt infections”. Indian Journal of Medical Microbiology 24.1 (2006): 52-54.
- Baradkar VP., et al. “Candida Infections of ventriculo-peritoneal shunts”. Journal of paediatric neuroscience 4.2 (2009): 73-75.
- Desai A., et al. “How long should cerebrospinal fluid cultures be held to detect shunt infections? Clinical article”. Journel of Neurosurgery: Pediatrics 4.2 (2009): 184-189.
- Jae-Joon Chung., et al. “Intraabdominal Complications Secondary to Ventriculoperitoneal shunts: CT Findings and Review of the Literature”. American journal of Roentgenology 193.5 (2009):1311-1317.
- Matthew J McGrit., et al. “Risk factors for paediatric Ventriculoperitoneal Shunt Infections and Predictors of Infectious Pathogens.” Clinical Infectious diseases 36.7 (2003): 858-862.
- Van Ende C., et al. “Intraperitoneal meropenum administration: a possible alternative to the intravenous route”. Peritoneal Dialysis International 30.2 (2010): 250-251.
- PJ Vlaar., et al. “Intraperitoneal compared Intravenous Meropenum for Peritoneal Dialysis-Related Peritonitis.” Journeal of the International Society for Peritoneal Dialysis 33.6 (2013): 708-709.
Citation:
Rezina Hamid., et al. “Alternate way to treat Ventriculo-Peritonitis”. Medical Research and Clinical Case Reports 2.3 (2018):
242-247.
Copyright: © 2018 Rezina Hamid., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.




































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.