Case Report
Volume 1 Issue 1 - 2017
Antenatal Diagnosis of Fetal Omphalocele and Preganancy Outcomes
Department of Gynecology-Obstetrics, Ibn Jazzar Hospital, Kairouan, Tunisia
*Corresponding Author: Fatnassi Ridha, Department of Gynecology and Obstetrics, Ibn El Jazzar Hospital, Kairouan, Tunisia.
Received: March 13, 2017; Published: July 20, 2017
Summary
The omphalocele is one of the most common fetal abdominal wall defects frequently associated with chromosomal abnormalities which determine prognosis. Early prenatal diagnosis is important for prognosis and for obstetric and neonatal management. We report three new cases of fetal omphaloceles accured in a 27, 43 and 39 years old patients. The diagnosis by the ultrasound exam was performed respectively at 12, 22 and 15 weeks of gestation. A fetal karyotype was performed to all the patients and was constantly abnormal. Therefore, the medical interruption of the pregnancy was practiced to all three patients. Risk factors, diagnosis, prognosis, management and pregnancy outcome are discussed referring to literature.
Keywords: Omphalocele; Abdominal wall defects; Antenatal diagnosis; Chromosomal analysis; Ultrasound
Introduction
Abdominal wall defects are congenital abnormalities including mainly gastroschisis and omphalocele. Omphalocele is an anterior abdominal defect with the herniated visceria covered by an amniotic-peritoneal membrane. The defect incidence ranges approximately between 1.5 and 3 per 10.000 births [1,2,3]. Most cases of omphaloceles are associated with serious abnormalities affecting negatively the prognosis [3]. The advent of prenatal ultrasonography allowed early detection of fetal omphalocele since 10-11th week of development [4]. Antenatal diagnosis of omphalocele can predict neonatal survival approaching and perinatal outcome. The treatment options vary from expectant management to surgical therapy [5].
Case 1
A 27 year old woman gravida 3 para 0 with a history of two spontaneous abortions, reported for routine antenatal ultrasound examination for the first time in the third month of pregnancy. There was no contributory family history of any congenital anomaly. Ultrasound showed 12 weeks of gestation and had identified an anterior abdominal wall defect with an extruded tissue mass measuring 1.3 cm in diameter (Figure 1). No other anomaly was noted in the foetus. Amniocentesis from chromosomal analysis was performed at 15 weeks of gestation and revealed a karyotype of 46, XX + 21. Pregnancy termination was decided and vaginal delivery was performed showing a male fetus with omphalocele and a cleft lip and palate.
A 27 year old woman gravida 3 para 0 with a history of two spontaneous abortions, reported for routine antenatal ultrasound examination for the first time in the third month of pregnancy. There was no contributory family history of any congenital anomaly. Ultrasound showed 12 weeks of gestation and had identified an anterior abdominal wall defect with an extruded tissue mass measuring 1.3 cm in diameter (Figure 1). No other anomaly was noted in the foetus. Amniocentesis from chromosomal analysis was performed at 15 weeks of gestation and revealed a karyotype of 46, XX + 21. Pregnancy termination was decided and vaginal delivery was performed showing a male fetus with omphalocele and a cleft lip and palate.
Figure 1: Prenatal ultrasonography at 12 weeks of gestation showing an anterior
abdominal wall defect with an extruded tissue mass measuring 1.3 cm in diameter.
Case 2
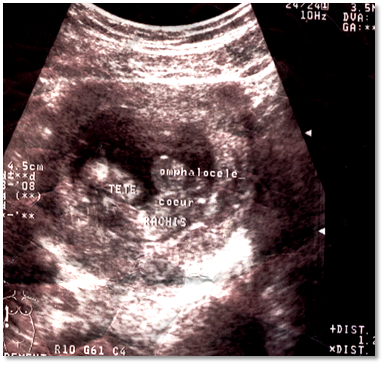
A 43 year old woman gravida 10 para 9 without previous medical and genetic history, presented for antenatal consultation in the sixth month of pregnancy with a large uteri. Ultrasound showed 22 weeks of gestation and had identified an anterior abdominal wall defect with an extruded tissue mass measuring 6 cm in diameter. The umbilical cord was inserted into the mass (Figure 2). Several other abnormalities were seen associating hydramnios and short limbs. The presence of omphalocele associated to micromelia was confirmed. Chromosome analysis revealed trisomy 18. Pregnancy termination was performed at 24 weeks of gestation showing a female fetus of 800g. Foetopathology examination revealed a giant omphalocele associated to multiple malformation syndrome characterized by short limbs, diaphragmatic defect, left heart hypoplasia and mitral stenosis. These abnormalities strongly suspected Cantrell pentalogy. Omphalocele was noted with bowel loops as its contents (Figure 3)
A 43 year old woman gravida 10 para 9 without previous medical and genetic history, presented for antenatal consultation in the sixth month of pregnancy with a large uteri. Ultrasound showed 22 weeks of gestation and had identified an anterior abdominal wall defect with an extruded tissue mass measuring 6 cm in diameter. The umbilical cord was inserted into the mass (Figure 2). Several other abnormalities were seen associating hydramnios and short limbs. The presence of omphalocele associated to micromelia was confirmed. Chromosome analysis revealed trisomy 18. Pregnancy termination was performed at 24 weeks of gestation showing a female fetus of 800g. Foetopathology examination revealed a giant omphalocele associated to multiple malformation syndrome characterized by short limbs, diaphragmatic defect, left heart hypoplasia and mitral stenosis. These abnormalities strongly suspected Cantrell pentalogy. Omphalocele was noted with bowel loops as its contents (Figure 3)
Case 3
A 39 year old woman gravida 3 para 2 was presented for our Department at 4 months gestation. Her family and personal medical and genetic history were negative. Ultrasonography was performed and showed a kinetic fetus with a crown-rump length consistent with 15 weeks’ gestation; a solid mass protruding from the ventral wall; choroid plexus cysts; and claw hands (Figure 4). The karyotype was obtained by amniocentesis and showed trisomy 18. Intrumental evacuation of uterine was performed at 16 weeks’ gestation showing a male fetus of 640g. Foetopathology examination confirmed the diagnosis of omphalocele associated to multiple malformation syndrome (Figure 5).
A 39 year old woman gravida 3 para 2 was presented for our Department at 4 months gestation. Her family and personal medical and genetic history were negative. Ultrasonography was performed and showed a kinetic fetus with a crown-rump length consistent with 15 weeks’ gestation; a solid mass protruding from the ventral wall; choroid plexus cysts; and claw hands (Figure 4). The karyotype was obtained by amniocentesis and showed trisomy 18. Intrumental evacuation of uterine was performed at 16 weeks’ gestation showing a male fetus of 640g. Foetopathology examination confirmed the diagnosis of omphalocele associated to multiple malformation syndrome (Figure 5).
Figure 5: Foetopathology examination showing a male fetus with an
omphalocele associated to a multiple malformation syndrome.
Discussion
Omphalocele is a one of the most congenital abdominal wall defects. The condition is described as an abnormal closure of the anterior abdominal wall causing a herniation of abdominal viscera into the base of the umbilical cord [1,2].
Several factors have been reported to increase the risks of omphalocele including positive family history of birth defect, chromosomal anomalies and history of spontaneous abortion as seen in case 1. There have been reports of an increased risk among males and twins. Although, maternal age is not considered as a risk factor, omphalocele is mostly associated with mothers being over 30 years [2]. Two of the patients reported in our study were over 30 years and fetus was male in two cases also.
The etiology of omphalocele is not clear and most is sporadic. Nevertheless, family cases is reported suggesting a genetically hypothesis [6]. Thanks to the advent of prenatal sonography, diagnosis of omphalocele is known feasible at as early as 12 weeks’ gestation. Ultrasonography is usually done for routine screening or during an investigation of elevated maternal serum alpha fetoprotein. It is showing a mass consisting of intra-abdominal contents witch herniated within a peritoneal sac into the amniotic cavity through a midline central defect at the base of umbilical insertion. Depending on the size of the defect, the sac can include bowel loops, liver, bladder, spleen, stomach, uterus, and ovaries [7].
Omphalocele is often associated with multiple other anomalies and chromosomal abnormalities which predict fetal prognosis and pregnancy outcome. It is associated in 14 to 47 % of cases with an elevated risk of cardiac defects especially in cases of normal karyotype. The central nervous anomalies are the second most frequently associated abnormality occurring in 3 to 33% of cases. Other abnormalities such as diaphragmatic defects, limb and urogenital anomalies, central nervous system anomalies also occurred commonly [6,8].
Trisomies 18 and 13 constitute the most genetic abnormalities accompanying omphalocele in 20-50% of cases. Multiple abnormalities can be associated and may be clustered in syndromic patterns mainly including cloacal exstrophy, Donnai-Barrow syndrome, pentalogy of Cantrell, and Beckwith-Wiedemann syndrome. This emphasizes the importance of an immediate and detailed search ultrasound examination and karyotyping once an omphalocele is identified [8]. In our study, two fetuses had trisomy 18. Of these, one fetus had Cantrell pentalogy.
Gastroschisis is considered as the major differential diagnosis of omphalocele. It is characterized by a full-thickness defect in the abdominal wall with no membranous covering and associated with normal umbilical cord insertion [6].
In cases of omphalocele, the overall mortality rate is ranging between 35 and 77% because of the high rate of medical abortion, spontaneous pregnancy loss and fetal demise [9]. Several studies noted that the prognosis changed when malformations were associated with omphalocele. In fact, when omphalocele was isolated, neonatal survival ranges between 50% and 90%. In contrast, when there were associated malformations or karyotype anomalies, mortality rate near to 100%. Associated anomalies allow prediction of neonatal morbidity and may affect the rate of terminations of pregnancy. No clear consensus has been done for the mode of delivery in fetuses with omphalocele. Nevertheless, caesarean section is frequently practised when the defect is large and in cases of higher risk of sac rupture and hepatic injury during delivery [9]. For ours three cases, pregnancy termination was decided by parents and performed because of the serious associated abnormalities.
Conclusion
Omphalocele is a common congenital abdominal wall defects with a high rate of mortality. Prognosis is affected often poor in cases of serious associated abnormalities. Prenatal diagnosis is feasible and easy since the first trimester and should be followed by karyotyping and a meticulous ultrasonography of the fetal. Pregnancy management depends on severity of associated defects. If pregnancy is allowed to progress, caesarean section should be contemplated mainly in case of a large defect and to prevent sac rupture.
References
- Curry JI., et al. “The aetiology of gastroschisis”. British Journal of Obstetrics and Gynaecology 107. 11 (2000): 1339-1346.
- Tan KH., et al. “Congenital anterior abdominal wall defects in England and Wales 1987–93: retrospective analysis of OPCS data”. BMJ 313.7069 (1996): 903-906.
- Rankin J., et al. “Congenital anterior abdominal wall defects in the north of England, 1986–1996: occurrence and outcome”. Prenatal Diagnosis 19.7 (1999) : 662-668.
- Liang YL., et al. “Prenatal diagnosis of fetal omphalocele by ultrasound: a comparison of two centuries”. Taiwanese Journal of Obstetrics and Gynecology 52.2 (2013): 258-263.
- JW Wladimiroff JC., et al. “Prenatal diagnosis and management of omphalocele”. European Journal of Obstetrics and Gynecology 16.1 (1983): 19-23.
- Daniel J Ledbetter. “Gastroschisis and Omphalocele”. Surgical Clinics of North America 86 (2006): 249-260.
- Prefumo F and Izzi C. “Fetal abdominal wall defects”. Best Practice & Research Clinical Obstetrics and Gynaecology (2012): 1-12.
- Gamba P and Midrio P. “Abdominal wall defects: Prenatal diagnosis, new born management, and long-term outcomes”. Seminars in Pediatric Surgery 23.5 (2014): 283-290.
- Tassin M., et al. “Omphalocele in the first trimester: prediction of perinatal outcome”. Prenatal Diagnosis 33.5 (2013): 497-501.
Citation:
Fatnassi Ridha., et al. “Antenatal Diagnosis of Fetal Omphalocele and Preganancy Outcomes”. Gynaecology and Perinatology
1.1 (2017): 39-43.
Copyright: © 2017 Fatnassi Ridha., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.