Short Communication
Volume 1 Issue 1 - 2016
Therapeutic Potential of Mechanical Protection of Pelvic Floor during Pregnancy
1Senior Lecturer, Faculty of Allied Health Professions, AIMST University, Semeling, 08100 Bedong, Kedah, Malaysia
*Corresponding Author: Yu Chye Wah, PhD, MSc, BSc. Senior Lecturer, Faculty of Allied Health Professions, Semeling, 08100 Bedong, Kedah, Malaysia.
Received: November 06, 2016; Published: December 12, 2016
Abstract
Birth trauma is generally be blamed for almost all the damage responsible for pelvic floor disorder (PFD). A study reveals that only half of pelvic floor damage among women who had vaginal delivery are due to birth trauma. Pelvic floor damage actually starts earlier, during the pregnancy itself due to normal physiological, hormonal and physical changes of pregnancy. Latest medical evidences show that mechanical pelvic floor support during defecation similar to perineal support during delivery, is found to greatly benefit various pelvic floor related disorders including anal fissure and hemorrhoid in pregnancy without medication. It is a promising option in prevention of PFD in the near future. It deserves serious attention from all medical practitioners.
Keywords: Pelvic floor; Pelvic floor disorder; Urinary incontinence; Constipation; Hemorrhoid
Introduction
A healthy pelvic floor is essential for normal functioning of pelvic organs that link to urinary, intestinal and reproductive system. Pelvic floor also plays an important role in continence and pelvic organ support [1]. However pelvic floor can be weakened by many causes, the most common causes include childbirth, and the associated straining of chronic constipation. The weakened pelvic floor may lead to PFD and manifests with symptoms of urinary incontinence (UI), pelvic organ prolapse (POP), constipation, sexual dysfunction, and associated problems like hemorrhoid [2,3]. Urinary incontinence (UI) is the involuntary loss of urine due to weakened pelvic floor support at bladder neck area [2]. Majority of constipation are obstructive type secondary to sagged pelvic floor [4,5]. Hemorrhoid is a venous dilatations of the hemorrhoidal plexus secondary to abnormal downward displacement of vascular anal cushions [6,7]. Repeated and prolonged straining during defecation, together with destructive changes in the supporting tissue of anal cushion worsen the engorgement of hemorrhoidal plexus [8].
It is an undeniable fact that PFD is due to weakened or damaged pelvic floor muscle. Its prevalence increases with aging and strongly associated with parity [9,10]. PFD is also strongly interrelated with chronic constipation in a vicious cycle [11] because as chronic straining during defecation will gradually cause descend pelvic floor, and this sagged pelvic floor with obstructed defecation lead to chronic constipation [12]. A study found constipation in women with UI correlates exclusively with posterior aspects of the pelvic floor support [13], and chronic constipation is a known risk for prolapse of pelvic organs and their recurrence [14,15].
Among all, birth trauma is the major causative factor for PFD [15] as birth trauma is associated with a variety of muscular and neuromuscular injuries of the pelvic floor that are linked to the development of urinary and anal incontinence, and pelvic organ prolapse [1]. Risk factors for pelvic floor injury include forceps delivery, episiotomy, prolonged second-stage of labor, and increased fetal size. Cesarean delivery appears to be protective, especially if the patient does not labor before delivery.
A study on 15,307 women revealed that women with vaginal deliveries as compared to cesarean sections had 1.7 times higher risk of UI. This study also found women who had cesarean sections as compared to nulliparous women had 1.5 times higher risk of UI [16].This clearly implies that half of the pelvic floor damage associated with parity is not due to vaginal delivery, but is actually caused during pregnancy itself.
The prevalence of UI, constipation and hemorrhoid are not only increased among women after delivery, in fact they start since the inception of pregnancy. A study on 43,279 women estimated the risk of UI during pregnancy increases two times more than before pregnancy [10]. Incidence of constipation and associated problems like haemorrhoid and anal fissure is significantly higher among women during pregnancy [17].
What could be the plausible reasons that cause the weakening of pelvic floor, besides the birth trauma? The following physiological changes occur during pregnancy:
- Elevated levels of circulating progesterone. Progesterone is an essential hormone for a healthy pregnancy. It brings about series of physiological changes in pregnant women. Pelvic floor muscles relax to get ready for smoother vaginal delivery. However raised progesterone may affect pelvic floor function, as it relaxes smooth muscles in the urinary system [18] and results in reduced ureter, bladder and urethral tone [19]. In addition, the increase of relaxin, a peptide hormone during pregnancy modifies the connective tissue by stretching the pelvic floor musculature and increases urethral pressure [20] and consequently this results in venous congestion and edema [21].
- Uterus size increases which leads to increased intra-abdominal pressure. Both the physiological changes in intra-abdominal pressure and heavy uterus will push pelvic floor downwards. This results in relaxation and sagging of pelvic floor, and subsequently contributes to obstructed defecation and causes more straining during defecation. With this repetitive straining, the pelvic floor is further pushed down and hemorrhoidal veins engorge to form hemorrhoid [6].
During the second stage of delivery, pelvic floor is exposed to trauma again by spontaneous tears, episiotomy or due to instrumentation. The trauma may require repair like episiotomy wound suture. The traumatized pelvic floor with or without repair continuously exposes to danger during defecation. During defecation, pelvic floor is pushed down 3 cm in normal person [21]. The downward push should be more with traumatized pelvic floor and during straining for constipation. The downward force, will stretch the fresh wound and prevent proper healing. Even though a small percentage may be diagnosed as wound dehiscence but majority may end up with permanent weakness of pelvic floor. This permanent weakened pelvic floor contributes to PFD and manifests in various PFD symptoms in later part of life.
What can be done to reduce the harm? Perineal support is a form of pelvic floor support routinely used during vaginal delivery to prevent damage of pelvic floor in second stage of delivery [22,23]. Even though there is a controversy in obstetric management between “hands off” and “hands poised” on the perineum as prevention to obstetric anal sphincter injuries (OASIS). However recent studies show perineal support by implementing a perineum protection training programme helps to reduce the incidence of OASIS [24,25]. On the other hand, anal fissure is the tear of anal mucosa mainly located at 6 o’clock position due to overstretching of anal mucosa during defecation [26]. Repeated stretching of anal mucosa as in chronic constipation prevent healing and gives rise to chronic anal fissure.
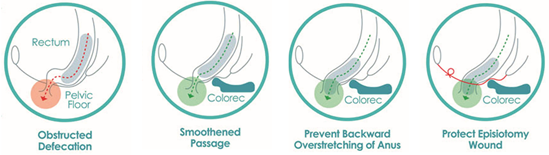
Based on similar concept with perineal support during delivery, bowel aid, a special toilet seat incorporates HPS (Hai’s perianal support) a protrusion to provide mechanical pelvic floor support during defecation has been proven to heal chronic anal fissure significantly [27,28]. In another study, the use of HPS with the same conservative supplementary pelvic floor support during defecation also found to effectively heal hemorrhoid in pregnancy without medication [29]. The therapeutic mechanisms of actions of HPS of bowel aid for pregnant women include, smoothen passage of defecation to benefit constipation and hemorrhoid, prevent backward overstretching of anus to avert anal fissure and prevent downward push to protect episiotomy wound (Figure 1).
Conclusion
PFD is widely believed to be due to vaginal delivery that causes damage of pelvic floor when pelvic floor is pushed downward and overstretched by baby going through vaginal orifice that traverses levator hiatus of pelvic floor. With the evidence shared above, it is obvious that pelvic floor damage actually starts during pregnancy, that is the reason why half of the risk of UI is related to spontaneous vaginal delivery. Based on similar concept of perineal support during vaginal delivery, HPS support during defecation to prevent downward push of pelvic floor and overstretching of anal mucosa when feces is forced through anal canal sharing the same levator hiatus as vagina, would has promising therapeutic benefit for pelvic floor. Practising bowel aided defecation with HPS during pregnancy may heal and prevent hemorrhoid, it would also minimize the damage of pelvic floor. Continual use of bowel aid with HPS in immediate post-natal period would allow better episiotomy wound healing and restoring better pelvic floor function. The supplementary support concept of bowel aided defecation for episiotomy wound is not totally new. It can be just comparable to using walking aid or crutches after orthopedic surgery of lower limb. Based on literature report and evidences collected so far, bowel aid may be useful to supplement the existing medical options for better prognosis in PFD prevention and management.
References
- Handa VL., et al. “Protecting the pelvic floor: obstetric management to prevent incontinence and pelvic organ prolapse”. Obstetrics & Gynecology 88.3 (1996): 470-478.
- Hunskaar S., et al. “The prevalence of urinary incontinence in women in four European countries”. BJU International 93.3 (2004): 324–330.
- Bump RC and Norton PA. “Epidemiology and natural history of pelvic floor dysfunction”. Obstetrics and Gynecology Clinics of North America 25.4 (1998): 723–746.
- Tinelli A., et al. “Age-related pelvic floor modifications and prolapse risk factors in postmenopausal women”. Menopause 17.1 (2010): 204-12.
- Maclennan AH., et al. “The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery”. An International Journal of Obstetrics & Gynecology 107.12 (2000): 1460–1470.
- Lohsiriwat V. “Hemorrhoids: From basic pathophysiology to clinical management”. World Journal of Gastroenterology 18.17 (2012): 2009-2017.
- Marieb EN. Hemorrhoids. In: Mallatt J, Wilhelm PB, editors. “Human Anatomy”. 4th ed. San Francisco, CA: Pearson Benjamin Cummings (2005): p. 530; 634.
- Abramowitz L., et al. “Haemorrhoidal disease in pregnancy”. Presse Médicale 40.10 (2011): 955-959.
- Kok G., et al. “Urinary Incontinence in Pregnant Women: Prevalence, Associated Factors, and Its Effects on Health-Related Quality of Life”. Journal of Wound Ostomy & Continence Nursing 43.5 (2016): 511-516.
- Wesnes SL., et al. “Urinary incontinence during pregnancy”. Obstetrics & Gynecology 109.4 (2007): 922-928.
- Berman L., et al. “Management of disorders of the posterior pelvic floor”. Yale Journal of Biology and Medicine 78.4 (2005): 211–221.
- Olsen AL and Rao SS. “Clinical neurophysiology and electrodiagnostic testing of the pelvic floor”. Gastroenterology Clinics of North America 30.1 (2001): 33–54. v-vi.
- Soligo M., et al. “Patterns of constipation in urogynecology: clinical importance and pathophysiologic insights”. American Journal of Obstetrics & Gynecology 195.1 (2006): 50-5.
- Kuncharapu I., et al. “Pelvic organ prolapse”. American Family Physician 81.9 (2010): 1111–1117.
- Jeon MJ., et al. “Risk factors for the recurrence of pelvic organ prolapse”. Gynecologic and Obstetric Investigation 66 (2008): 268–273.
- Rortveit G., et al. “Urinary incontinence after vaginal delivery or cesarean section”. The New England Journal of Medicine 348.10 (2003): 900-907.
- Poskus T., et al. “Haemorrhoids and anal fissures during pregnancy and after childbirth: a prospective cohort study”. An International Journal of Obstetrics and Gynaecology 121.13 (2014): 1666-71.
- Swift SE and Ostergard DR. “Effects of progesterone on the urinary tract”. International Urogynecology Journal 4.4 (1993): 232–236.
- Tincello DG., et al. “Second trimester concentration of relaxin and pregnancy related incontinence”. European Journal of Obstetrics & Gynecology and Reproductive Biology 106.2 (2003): 237–238.
- Hilton P and Dolan LM. “Pathophysiology of urinary incontinence and pelvic organ prolapse”. An International Journal of Obstetrics and Gynaecology 111. sup.1 (2004): 5–9.
- Singer AJ and Brandt LJ. “Pathophysiology of the gastrointestinal tract during pregnancy”. The American Journal of Gastroenterology 86.12 (1991): 1695-1712.
- Apostolis C., et al. “Assessment of women with defecatory dysfunction and manual splinting using dynamic pelvic floor magnetic resonance imaging”. Female Pelvic Medicine & Reconstructive Surgery 18.1 (2012): 18-24.
- National Institute for Health and Clinical Excellence. “Intrapartum care: Care of healthy women and their babies during childbirth”. NICE clinical guideline 55. Manchester: NICE; 2007.
- Hals E., et al. “A multicenter interventional program to reduce the incidence of anal sphincter tears”. Obstetrics & Gynecology 116.4 (2010): 901–908.
- Laine K., et al. “Incidence of obstetric anal sphincter injuries after training to protect the perineum: cohort study”. BMJ Open 2.5 (2012): e001649.
- Poh A., et al. “Innovation in Chronic Anal Fissure Treatment: A systematic review”. World Journal of Gastrointestinal Surgery 2.7 (2010): 231–241.
- Gee T., et al. “Ano-coccygeal support in the treatment of idiopathic chronic posterior anal fissure: a prospective non-randomised controlled pilot trial”. Techniques in Coloproctology 17.2 (2013): 181-6.
- Tan KY., et al. “Posterior perineal support as treatment for anal fissures-preliminary results with a new toilet seat device”. Techniques in Coloproctology 13.1 (2009): 11-15.
- Lim SS., et al. “Comparing topical hydrocortisone cream with Hai’s Perianal Support in managing symptomatic hemorrhoids in pregnancy: a preliminary trial”. The journal of obstetrics and gynaecology research 41.2 (2015): 238-247.
Citation:
Yu Chye Wah and Chew Heng Hai. “Therapeutic Potential of Mechanical Protection of Pelvic Floor during Pregnancy”. Gynaecology
and Perinatology 1.1 (2016): 18-21.
Copyright: © 2016 Yu Chye Wah and Chew Heng Hai. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.