Research Article
Volume 2 Issue 6 - 2018
Infra-Mammary Incision versus Peri-Areolar Incision in Management of Large Benign Breast Lesions; a Novel Approach
1Lecturer of General surgery, Faculty of Medicine, Zagazig
2Lecturer of General surgery, Faculty of Medicine, Zagazig University
3Assistant professor of General surgery, Faculty of Medicine, Zagazig
4Assistant lecturer of Internal medicine department, Faculty of Medicine, Zagazig University
2Lecturer of General surgery, Faculty of Medicine, Zagazig University
3Assistant professor of General surgery, Faculty of Medicine, Zagazig
4Assistant lecturer of Internal medicine department, Faculty of Medicine, Zagazig University
*Corresponding Author: Loay M Gertallah, Department of General Surgery, Zagazig university faculty of medicine Egypt.
Received: August 16, 2018; Published: September 04, 2018
Abstract
Objective: The usual surgical approach for excision of benign breast lesions leaves permanent scars which affect the cosmetic appearance of the breast. Peri-areolar incision is generally considered the main incision used for excision of benign breast lesions. But such incision might have some drawbacks e.g. loss of nipple sensation, skin necrosis and loss.
The current study aims to evaluate the novel infra-mammary incision for surgical excision of benign breast lesions as regard postoperative complications and patients cosmetic satisfaction.
Patients and Method: Thirty patients with different types of benign breast lesions were included in our prospective study, patients were divided into 2 groups; each group contains 15 patients. We performed infra-mammary incision for management of the first group (group A) and peri-areolar incision for management of the 2nd group (group B).
Results: We have found that the group of patients which was managed by infra-mammary incision the postoperative hospital stay was shorter, nipple sensation was preserved and intact in all patients and during follow up visits all patients were cosmetically satisfied by the result of surgery. Statistically significant differences were found between both groups regarding all these parameters.
Conclusion: the infra-mammary approach is better than the peri-areolar approach for management of large fibroadenoma, mammary cystic hyperplasia and gynecomastia since it can achieve excision of the lesion while preserving nipple sensation and vascularity, so it is associated with a higher patient's satisfaction.
Keyword: Infra-mammary approach; Peri-areolar approach; Benign breast lesions; Patient's satisfaction
Introduction
Breast lesions could markedly affect the psychological and physical health of women. Recently, incidence of benign and malignant breast tumors was rising. Benign breast lesions are more common than malignant breast tumors, forming about > 90% of patients that were referred to health care centers [1 & 2]. Benign breast lesions include fibroadenoma, intra-ductal papilloma, mammary cystic hyperplasia, mammary duct ectasia and traumatic fat necrosis. Fibroadenomas are the commonest and most commonly occur in females' ages 15–30 years [3]. Surgical resection is the main therapeutic method for management of those lesions, to confirm the diagnosis, to exclude malignancy and to avoid malignant occurrence later on [4]. Moreover, surgical excision is considered the definitive management for symptomatic benign breast tumors to relief patients' anxiety as regard liability for more growth or malignant transformation as well as physical discomfort [5]. As the risk of transformation of most benign breast lesions is low so the main goal of management of such lesions is clinical cure with preservation of the cosmetic appearance of the breast and sensation of the nipple.
Mammary duct ectasia is a chronic inflammation and dilatation of the breast ducts and surrounding tissues, which it may be presented with an indurated mass underneath the areola which might resemble carcinoma [6 & 7]. Its main treatment is with antibiotic therapy but in cases with a large mass, surgical management is the best treatment option to allow radical treatment and to exclude malignancy [8]. Worldwide, peri-areolar incision is considered the main surgical approach for management of most benign breast lesions. But such procedure has many drawbacks as the loss of nipple sensation and disturbed vascularity as a result of nerve cutting and impaired blood supply of the nipple and areola [9]. In the current study we have described a novel minimally invasive approach for the surgical management of benign breast lesions which is the infra-mammary approach. We hypothesized that the infra-mammary approach will be better than the peri-areolar approach regarding cosmetic appearance and preservation of the nipple sensation.
This current study aims to evaluate the novel benefits of infra-mammary incision for surgical excision of benign breast lesions as regard postoperative complications and patients cosmetic satisfaction.
Patients & Methods
Study design:
- This is a prospective cohort study that was done in department of General Surgery, Faculty of Medicine Zagazig University.
- Sample size: our study included 30 patients with different subtypes of breast masses which were clinically and radiologically are found to be benign. We divided them into 2 groups; group A and group B each group contain 15 patients each group includes 13 females and 2 males with gynecomastia. All patients were operated for surgical excision of the breast lesion. We performed infra-mammary incision for surgical management of the group A and peri-areolar incision for surgical management of group B.
- Patient's data: Table 1
- We included 26 female patients and 4 male patients with gynecomastia
- Our patients age range from 15-40 years old.
- All the 30 patients are diagnosed with benign breast lesions and have no serious comorbid conditions.
Preoperative preparation
All patients were subjected to the following:
All patients were subjected to the following:
- Full history taking.
- Complete local and general clinical examination.
- Preoperative investigations:
- C.B.C.
- Live & renal function tests
- Plain X-ray chest
- Breast mammography
Operative details
Group: A
Group: A
- Before general anesthesia, the infra-mammary region and the lesion were labeled while the patient was standing. Prophylactic preoperative antibiotic treatment (100 ml metronidazol and 1, 2 gm amoxicillin and clavulonic acid were given to all included patients in our study.
- Patients were placed in the supine position with both her arms fully abducted. The whole breast was sterilized by using povidine iodine and the incision was made in the infra-mammary fold.
- Breasts’ skin was pulled upward and main breast tissue was compressed downward and diathermy sharp dissection was done through the breast tissue until reaching the lesion.
- The lesion was dissected by a scissor with the help of traction and counter traction between the breast skin and the duct system.
- We end the operation by inserting a vacuum suction drain in the breast tissue followed by making proper hemostasis, closure of infra-mammary incision by subcutaneous stitches and then closure of the skin by subcuticular stitches.
Group: B
- The usual peri-areolar incision was done. We made an incision at the areolar border and the nipple where the areola skin flap is raised until we have reached the lesion and excising it.
Postoperative follow up
We have followed our patients in the early postoperative period for the following:
We have followed our patients in the early postoperative period for the following:
- Length of hospital stays (1-2 days).
- Early wound infection or ischemia or seroma.
- Post-operative pain, nipple sensation or nipple necrosis.
- Evaluation of the postoperative pain was done by assessment of the average consumption of analgesic ampules given on patient demand during the first week.
- All patients received a routine intramuscular dose of 75-mg dose of diclophenac sodium (Voltaren IM; Novartis, Basel, Switzerland) twice on the day of the operation.
- Oral intake was allowed after 3 hours postoperatively. Treatment was removed after delivering less than 20cc serous fluid.
- Most patients were discharged a day after the operation. We have sent excised specimen histopathology.
- The patients were followed-up postoperatively daily until discharge from the hospital, then 2 times in the week in the outpatient clinic for the first 2 weeks, then once monthly later on, and finally every 6 month.
- The patients were followed-up postoperatively daily until discharge from the hospital, then 2 times in the week in the outpatient clinic for the first 2 weeks, then once monthly later on, and finally every 6 month.
- Postoperative scar, nipple sensation and vascularity, skin complication and over all patient satisfaction were recorded at every visit.
Statistical analysis
Data of the patients were computerized and analyzed statistically using SPSS program (Statistical Package for Social Science). Chi square test (χ2) and Independent T test was used to calculate difference between qualitative variables. P-value ≤ 0.05 is considered a significant difference, p < 0.001 is considered a highly significant difference while, P > 0.05 is considered non-significant difference.
Data of the patients were computerized and analyzed statistically using SPSS program (Statistical Package for Social Science). Chi square test (χ2) and Independent T test was used to calculate difference between qualitative variables. P-value ≤ 0.05 is considered a significant difference, p < 0.001 is considered a highly significant difference while, P > 0.05 is considered non-significant difference.
| Surgical Procedure | P | |||||
| Peri-areolar Incision N = 15 | Infra-mammary Incision N = 15 | |||||
| Age, Years* | Mean ± SD | 32.13 ± 9.51 | 33.47 ± 7.56 | 0.674 | ||
| N | % | N | % | |||
| Sex | F | 13 | 86.7% | 13 | 86.7% | 1 |
| M | 2 | 13.3% | 2 | 13.3% | ||
| Comorbid Condition | No | 12 | 80.0% | 10 | 66.7% | 0.409 |
| Yes | 3 | 20.0% | 5 | 33.3% | ||
Table 1: The clinico-demographic data of both groups.
All variables were compared using Chi-square X2 test except (*) Independent T
All variables were compared using Chi-square X2 test except (*) Independent T
Results
Preoperative and operative results
This study was performed on 26 female patients suffering from different benign breast lesions and 4 male patients suffering from gynecomastia which need surgical excision. 15 of them; 13 females and 2 males, were managed by infra-mammary approach (group A) and 15 of them 13 females and 2 males, were managed by Peri-areolar incision (Group B). The clinico-demographic data of all patients were included in (Table 2).
This study was performed on 26 female patients suffering from different benign breast lesions and 4 male patients suffering from gynecomastia which need surgical excision. 15 of them; 13 females and 2 males, were managed by infra-mammary approach (group A) and 15 of them 13 females and 2 males, were managed by Peri-areolar incision (Group B). The clinico-demographic data of all patients were included in (Table 2).
| Surgical Procedure | P | |||||
| Peri-areolar Incision N = 15 | Infra-mammary Incision N=15 | |||||
| Size of The Excised Lesion by Cm* | Mean ± SD | 4.7±1.2 | 4.7±1.2 | 1 | ||
| N | % | N | % | |||
| Size of The Excised Lesion by Cm | 3 cm | 6 | 26.7% | 2 | 26.7% | 0.011 |
| 4 cm | 5 | 26.7% | 2 | 26.7% | ||
| 5 cm | 3 | 20.0% | 5 | 20.0% | ||
| 6 cm | 1 | 26.7% | 6 | 26.7% | ||
| Histological Diagnosis of The Excised Lesion | Fibroadenoma | 3 | 20.0% | 4 | 26.7% | 0.055 |
| Fibrocystic | 5 | 33.3% | 3 | 20.0% | ||
| Major Duct Papilloma | 5 | 33.3% | 0 | 0.0% | ||
| Duct Ectasia | 1 | 6.7% | 4 | 26.7% | ||
| TFN | 1 | 6.7% | 4 | 26.7% | ||
| Location of The Lesion | Upper Medial | 2 | 13.3% | 1 | 6.7% | 0.017 |
| Lower Medial | 1 | 6.7% | 6 | 40% | ||
| Upper Lateral | 5 | 13.3% | 1 | 6.7% | ||
| Lower Lateral | 1 | 26.7% | 6 | 40% | ||
| Central | 6 | 40.0% | 1 | 6.7% | ||
| Number of Lesions | Single | 12 | 80.0% | 13 | 86.7% | 0.624 |
| Multiple | 3 | 20.0% | 2 | 13.3% | ||
| Yes | 11 | 73.3% | 15 | 100.0% | ||
Table 2: Comparison of clinico-pathological data of both groups.
All variables were compared using Chi-square X2 test except (*) Independent T
All variables were compared using Chi-square X2 test except (*) Independent T
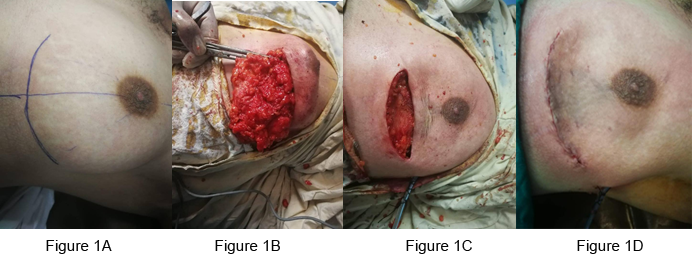
Figure 1: Infra-mammary approach in management of a male patient with gynecomastia.
A) Preoperative labeling of site of the incision
B) B excision of the lesion
C) C after excision of the lesion
D) D closure of the incision after excision of the lesion
A) Preoperative labeling of site of the incision
B) B excision of the lesion
C) C after excision of the lesion
D) D closure of the incision after excision of the lesion
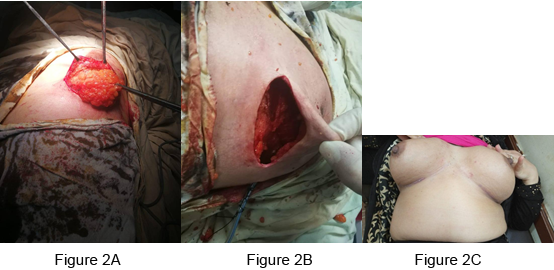
Figure 2: Infra-mammary approaches in management of a female patient with a large fibroadenoma.
A) Excision of the lesion
B) After excision of the lesion
C) Post-operative appearance of the incision after healing
A) Excision of the lesion
B) After excision of the lesion
C) Post-operative appearance of the incision after healing
There is statistically significant differences between both groups regarding the size of the lesion (p = 0.011), which denotes that infra-mammary approach is more suitable for large lesions while peri-areolar approach is better for small lesions.
There is a statistically significant differences between both groups regarding the location of the lesion with in the breast quadrants (p = 0.017), which denotes that infra-mammary approach is more suitable for lesions which are located in the lower medial and lateral quadrants while peri-areolar approach is better for upper medial and lateral quadrants.
No statistically significant differences were found between both groups regarding the age, sex of the patient or histopathological subtype or number of the lesions. (Table 2)
The intraoperative time ranged from 35 to 65 minutes with a mean operative time of 50 minutes. No statistically significant differences between both groups regarding the length of operative time. No intraoperative complications occurred and none of the patients needed blood transfusion.
Postoperative results
There is a statistically significant difference between both groups regarding the length of hospital stay (p = < 0.001), presence of sensory affection of the nipple (p = 0.048), presence of vascular affection of the nipple (p = 0.039) presence of post-operative complications and cosmetic satisfaction of the patients (p = 0.32) which denotes that infra-mammary approach is better that peri-areolar approach regarding those findings. Table 3 No mortality related to the operation was recorded in all cases.
There is a statistically significant difference between both groups regarding the length of hospital stay (p = < 0.001), presence of sensory affection of the nipple (p = 0.048), presence of vascular affection of the nipple (p = 0.039) presence of post-operative complications and cosmetic satisfaction of the patients (p = 0.32) which denotes that infra-mammary approach is better that peri-areolar approach regarding those findings. Table 3 No mortality related to the operation was recorded in all cases.
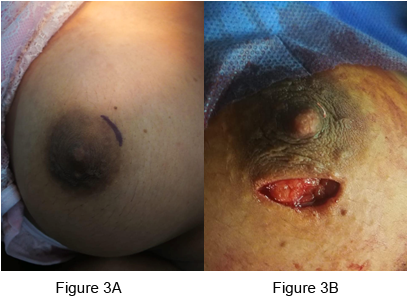
Figure 3: Peri-areolar approach in management of a female patient
with a small fibroadenoma A Preoperative Labeling of site of the incision
B performing an incision for excision of the lesion
| Surgical Procedure | P | |||||
| Peri-areolar Incision N = 15 | Infra-mammary Incision N=15 | |||||
| Duration Of Hospital Stay In Days | 1 | 0 | 0.0% | 15 | 100.0% | < 0.001 |
| 2 | 4 | 26.7% | 0 | 0.0% | ||
| 3 | 6 | 40.0% | 0 | 0.0% | ||
| 4 | 5 | 33.3% | 0 | 0.0% | ||
| Second Admission | No | 13 | 86.7% | 15 | 100.0% | 0.043 |
| Yes | 2 | 13.3% | 0 | 0.0% | ||
| Complications | No | 11 | 73.3% | 15 | 100.0% | 0.032 |
| Yes | 4 | 26.7% | 0 | 0.0% | ||
| Sensory Affection Of The Nipple | No | 13 | 86.7% | 15 | 100.0% | 0.048 |
| Yes | 2 | 13.3% | 0 | 0.0% | ||
| Vascular Affection Of The Nipple | No | 13 | 86.7% | 15 | 100.0% | 0.039 |
| Yes | 2 | 13.3% | 0 | 0.0% | ||
| Superficial Ischemia | No | 13 | 86.7% | 15 | 100.0% | 0.050 |
| Yes | 2 | 13.3% | 0 | 0.0% | ||
| Painful Ugly Scar | No | 13 | 86.7% | 15 | 100.0% | 0.143 |
| Yes | 2 | 13.3% | 0 | 0.0% | ||
| Technical& Clinical Success (Complete Cure Without Complications | No | 2 | 13.3% | 0 | 0.0% | 0.143 |
| Yes | 13 | 86.7% | 15 | 100.0% | ||
| Patient Cosmotic Satisfaction | No | 4 | 26.7% | 0 | 0.0% | 0.032 |
| Yes | 11 | 73.3% | 15 | 100.0% | ||
Table 3: Comparison of operative and post-operative details of both groups.
All variables were compared using Chi-square X2 test except (*) Independent T
All variables were compared using Chi-square X2 test except (*) Independent T
Discussion
Generally, conservative management cannot lead to radical cure of most benign breast lesions, and surgical excision is the most effective and sure line of treatment. There are many forms of traditional incisions for benign breast lesions e.g. radial incisions along the skin above the pathological lesion of the breast. Such surgery is easy but it carries the risk of obvious scarring which affects the cosmetic appearance of the breast seriously, especially, in patients with multiple lesions. Nowadays, the requirement for a beautiful breast appearance post-operatively is of higher value, as the lesions are benign so the main aim of surgery is to remove the lesion with preservation of the cosmetic appearance of the breast and sensation of the nipple [4].
Hadfield’s operation was the classic treatment approach of management of such lesions [10]. The classical Hadfield’s approach is characterized by making an incision at the areolar border and the nipple, then the areola skin flap is raised and the entire lesion is excised [11].
But this approach is associated with diminished nipple sensation and nipple anesthesia in most patients in addition to nipple/areola necrosis in some patients and, recurrent sepsis may take place in some cases [9 & 12].Studying the pattern of blood and nerve supply of the nipple and areola complex helped in understanding the reasons of diminished nipple sensation and necrosis of the nipple and areola which are associated with per-areolar approach. We performed such study to prove the benefits of infra-mammary incision more than the peri-areolar incision in management of benign breast lesions regarding clinical cure and patients' satisfaction patients who underwent infra-mammary incision did not suffer from postoperative nipple loss of sensation or necrosis, as infra-mammary incision avoid raising areolar skin flap which lead to impaired sensation and vascularity of the nipple in case of per-areolar approach, our results are similar to results of Reda., et al. [8], who used the infra-mammary approach to manage mammary duct ectasia only but in the current study we have widened its use to manage other benign breast lesion. The benefit of the infra-mammary approach is that cutting of the subdermal nerve plexus and subcutaneous blood vessels which supply the nipple areola area was avoided.
Ciftci., et al. [13] stated that most breast masses might be removed by peri-areolar incision except for giant lesions. That was in line with our results that infra-mammary is better in management of large benign lesions. Reda., et al. [8], have used the infra-mammary approach and it enabled them to dissect the whole duct system completely with complete vision from underneath the nipple down to the pectoral fascia and moreover such approach allowed us to remove all different lesions with variable size completely without leaving any remnants and so lead to decreased the risk of residual lesion. This explains the absence of recurrent disease in all included cases in our study. In the current study such approach allows excision of any benign lesion with high technical success and with the maximum patients' satisfaction without recurrence or cosmetic affection.
In Reda., et al. [8], study, the overall patients’ satisfaction was around 95% and in our study was 100% since the main pathology was treated with the best breast shape including nipple projection and hidden scar without postoperative complication. The periareolar incision was used widely in management of gynecomastia [14 & 15], and in breast augmentation [16 & 17], for a long time because of its many cosmetic advantages. Previously, surgeons considered the periareolar incision as the gateway to the breast [18]. All these previous studies are in line with our study. Different results were found by Tiryaki., et al. [19],that cosmetic results were satisfactory for young patients with palpable fibroadenoma who had undergone operation by a peri-areolar incision.
In line with our results;Liu., et al. [20],stated that peri-areolar incision has many drawbacks, the operation time was longer, and the volume of intraoperative blood loss was larger when compared with the infra-mammary approach and these problems are essential as refinement of surgical techniques which includes exposure, hemostasis, and closure is required for surgeons. Also,Liu., et al. Araco., et al.and Benediktsson., et al.stated there was a risk of nipple sensation loss in case of peri-areolar incision [20-22]. Also,Liu., et al. [20],described another disadvantage of the peri-areolar incision carries the risk of disruption of lactation and it may interrupt milk ducts. Another major disadvantage of the peri-areolar incision is that is an increased tendency for Caribbean women to develops hypertrophic scars and keloids [23]. All these results are in line with our results that infra-mammary approach is better without apparent dis advantages.
Kong., et al.2016 proved different results from us and they encourage performing peri-areolar incision in management of benign breast lesions as the skin of the areola area is thin, and it has good elasticity and strength. Moreover, post‑operative scar is not obvious and can quickly heal.
Kong., et al. [4], found no obvious scarring and patient satisfaction was high at 98%, and due to its cosmetic role they suggest the peri-areolar incision as a perfect approach for management of gynecomastia which was in line with previous studies [24-26]. These different are different from our results.
Other studies have reported that there are no differences between both peri-areolar and infra-mammary incisions with regard to the duration of surgery or the amount of intra-operative bleeding [27 & 28].
Kong., et al. [4], described that there are disadvantage of the peri-areolar incision e.g. it causes more damage to the subcutaneous tunnel and mammary tissues, so it requires more focus on the surgical techniques, like intraoperative exposure, bleeding and incision closure, or the risk of surgical complications increase. They found 2 (1.3%) patients developed nipple ischemia that is inline without results as we found some cases of nipple ischemia but in infra-mammary approach no ischemia or loss of nipple sensation were detected in any case.
It has previously been reported that a peri-areolar incision is not suitable when the diameter of the tumor is > 5 cm or when the space between the tumor and the areola is > 3‑4 cm, as the surgery would cause significant damage to the lactiferous ducts [29]. However, in our study, an infra-mammary incision was used even when the distance between the tumor and the areola was 7.5 cm to ensure good patient outcomes.
In contrast to our results Naraynsingh., et al. [3], stated that the infra-mammary approach may lead to an apparent scar mainly in the young breast that is not pendulous. Moreover they proved that infra-mammary incisions for tumors in the upper half of the breast require dissection through or around more breast tissue that will be associated with unnecessary damage to the normal breast tissue.
Conclusion
Benign breast lesions are increasing in incidence the surgical excision of them is the main line of management, due to the benign nature of most breast lesion the most important parameter is preserving the cosmetic appearance of the breast we have compared the infra-mammary incision with the peri-areolar incision in management of such lesions and we have found that the infra-mammary approach is better than the per-areolar regarding lower risk of inrta- and peri-operative complications, preserved nipple sensation and vascularity additionally infra-mammary incision brings hope to female patients with benign breast lesions as it enables the cure of the disease with maintaining the appearance of the breast. Moreover it provides a quick recovery, hidden incision, and small scar. So it is associated with preserved sensory nerve supply and the blood supply of the nipple and areola complex with the normal appearance and projection of the nipple so, it is associated with a higher patients satisfaction.
The peri-areolar incision that was the main surgical approach of management of benign breast lesions requires more technical requirements from the surgeons and it may lead to areola collapse. From the point of the cosmetic appearance of the breast, we advise patients with high cosmetic requirements to order infra-mammary incision to maintain a good breast shape.
Authors declared no conflict of interest
References
- Chen W., et al. “The incidences and mortalities of major cancers in China, 2009”. Chinese Journal of Cancer 32 (2013): 106-112.
- Onstad M and Stuckey A. “Benign breast disorders”. Obstetrics & Gynecology Clinics of North America 40 (2013): 459-473.
- Naraynsingh V., et al. “The ‘Saw Tooth’ operation for giant fibroadenomas”. International Journal of Surgery Case Reports 41 (2017): 304-306.
- KONG X., et al. “Periareolar incision for the management of benign breast tumors”. ONCOLOGY LETTERS 12 (2013): 3259-3263.
- Lakoma A and Kim E. “Minimally invasive surgical management of benign breast lesions”. Gland Surgery 3.2 (2014): 142-148.
- Dogan BE., et al. “Ductal dilatation as the manifesting sign of invasive ductal carcinoma”. Journal of Ultrasound in Medicine 24 (2005): 1413-1417.
- Duchesne N., et al. “Ultrasound appearance of chronic mammary duct ectasia”. Canadian Association of Radiologists Journal 56 (2005): 297-300.
- Reda AA., et al. “Infra Mammary Approach for Major Duct Excision in the Management of Multiple Duct Ectasia: Our First Steps”. Surgery: Current Research 6 (2016): 273.
- Chapman D., et al. “Postoperative complications following sub areolar duct clearance”. Cancer Nursing Practice 5 (2006): 36-39.
- Lanitis S., et al. “Microdochectomy for singleduct pathologic nipple discharge and normal or benign imaging and cytology”. Breast 17 (2008): 309-313.
- Harris JR., et al. Management of common breast disorders. Breast Diseases. (1987).
- Srivastava A., et al. “A safe technique of major mammary duct excision”. Journal of the Royal College of Surgeons of Edinburgh 40 (1995): 35-37.
- Ciftci I., et al. “Inframammarial Giant Fibroadenoma Removing and a Nipple-sparing Breast Reconstruction in an Adolescent: A Case Report” Prague Medical Report 116. 2 (2015): 161-166.
- Saad MN and Kay S. “The circumareolar incision: a useful incision for gynecomastia”. Annals of the Royal College of Surgeons of England 66.2 (1984): 121-122.
- Pitanguy I. “Transareolar incision for gynecomastia”. Plastic and Reconstructive Surgery 38.5 (1966): 414-419.
- Becker H. “The intra-areolar incision for breast augmentation”. Annals of Plastic Surgery 42.1 (1999): 103-106.
- Jones FR and Tauras AP. “A periareolar incision for augmentation mammaplasty”. Plastic and Reconstructive Surgery 51.6 (1973): 641-644.
- Shrotria S. “The peri-areolar incision--gateway to the breast!”. European Journal of Surgical Oncology 27.6 (2001): 601-603.
- Tiryaki T., et al. “Breast fibroadenoma in female adolescents”. Saudi Medical Journal 28.1 (2007): 137-138.
- Liu XF., et al. “A clinical study on the resection of breast fibroadenoma using two types of incision”. Scandinavian Journal of Surgery 100 (2011): 147-152.
- Araco F., et al. “Sensitivity of the nipple-areola complex and areola pain following aesthetic breast augmentation in a retrospective series of 1200 patients: periareolar versus sub-mammary incision”. Plastic and Reconstructive Surgery 128.4 (2011): 984-989.
- Benediktsson KP., et al. “Touch sensibility in the breast after subcutaneous mastectomy and immediate reconstruction with a prosthesis”. British Journal of Plastic Surgery 50.6 (1997): 443- 449.
- V Naraynsingh., et al. “Swiss-roll operation for giantfibroadenomas”. The Breast Journal 8.1(2002): 45-46.
- Lapid O., et al. “Gynaecomastia surgery in the Netherlands: What, why, who, where”. Journal of Plastic, Reconstructive & Aesthetic Surgery 67 (2014): 702-706.
- Lee JH., et al. “Surgical correction of gynecomastia with minimal scarring”. Aesthetic Plastic Surgery 36 (2012): 1302-1306.
- Cannistra C., et al. “Surgical treatment of gynecomastia with severe ptosis: Periareolar incision and dermal double areolar pedicle technique”. Aesthetic Plastic Surgery 33 (2009): 834-837.
- Chen XY. “Clinical observation on surgery through a minimal incision around areola mammae in treatment of benign tumor of mammary glands”. Oncology Letters 20 (2014): 777-780.
- Hu N. “The clinical effects of different resection type of breast Fibroids”. Zhongguo YIyao Daokan 15 (2013): 1135-1137.
- Zhao XY. “Application value of areola incision at the edge of the benign breast tumor resection”. Zhongguo Shiyong Yiyao 5 (2010): 57-58.
Citation:
Loay M Gertallah., et al. “Infra-Mammary Incision versus Peri-Areolar Incision in Management of Large Benign Breast Lesions;
a Novel Approach”. Chronicle of Medicine and Surgery 2.6 (2018): 281-290.
Copyright: © 2018 Loay M Gertallah., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.